Megacolon occurs when part of the colon becomes abnormally enlarged, often leading to slow or blocked bowel movements, which can result in intestinal obstruction. This condition causes symptoms like severe constipation, abdominal pain, and swelling, requiring timely diagnosis and treatment to prevent complications. Discover how understanding the causes and treatments can help you manage these digestive challenges effectively by reading the rest of the article.
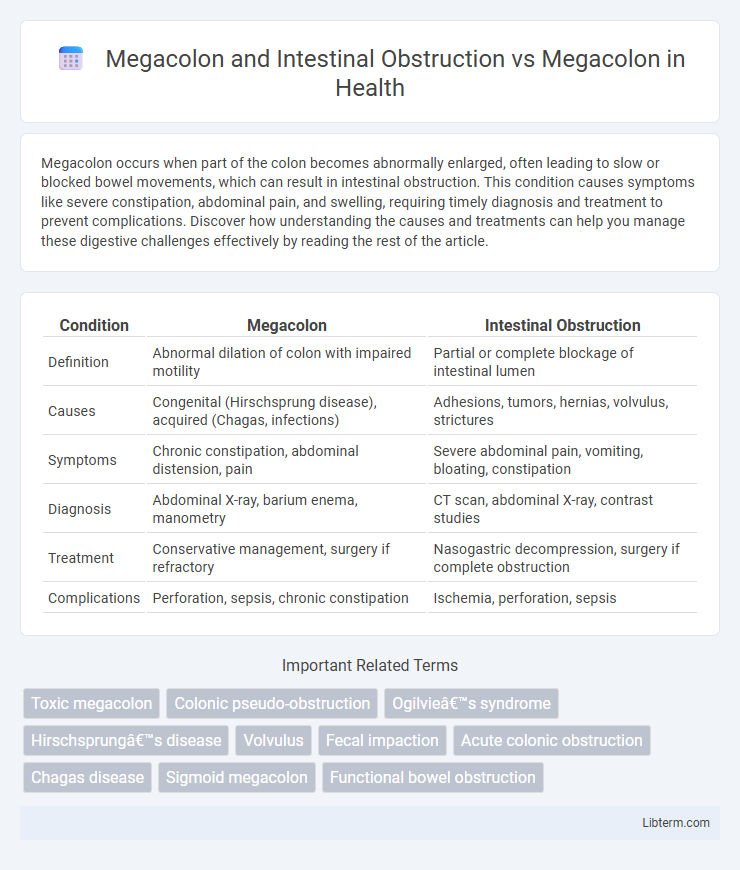
Table of Comparison
| Condition | Megacolon | Intestinal Obstruction |
|---|---|---|
| Definition | Abnormal dilation of colon with impaired motility | Partial or complete blockage of intestinal lumen |
| Causes | Congenital (Hirschsprung disease), acquired (Chagas, infections) | Adhesions, tumors, hernias, volvulus, strictures |
| Symptoms | Chronic constipation, abdominal distension, pain | Severe abdominal pain, vomiting, bloating, constipation |
| Diagnosis | Abdominal X-ray, barium enema, manometry | CT scan, abdominal X-ray, contrast studies |
| Treatment | Conservative management, surgery if refractory | Nasogastric decompression, surgery if complete obstruction |
| Complications | Perforation, sepsis, chronic constipation | Ischemia, perforation, sepsis |
Understanding Megacolon: Definition and Types
Megacolon refers to an abnormal dilation of the colon, which can be classified into congenital, idiopathic, and acquired types. Intestinal obstruction is a potential complication of megacolon, occurring when the dilated colon impedes the normal passage of intestinal contents. Understanding the differences between megacolon alone and megacolon with intestinal obstruction is crucial for accurate diagnosis and effective treatment planning.
What is Intestinal Obstruction? An Overview
Intestinal obstruction is a blockage that prevents the normal passage of contents through the intestines, often caused by mechanical factors like tumors, adhesions, or impacted stool. Megacolon, an abnormal dilation of the colon, can result from or contribute to intestinal obstruction, leading to symptoms such as severe abdominal distension and constipation. Differentiating between primary megacolon and obstruction is crucial for treatment, as obstruction often requires urgent intervention to relieve the blockage and prevent complications.
Causes of Megacolon: Primary vs Secondary
Megacolon arises from either primary causes, such as congenital conditions like Hirschsprung's disease where nerve cells are absent in parts of the colon, or secondary causes including infections, inflammatory diseases, or chronic constipation leading to functional obstruction. Intestinal obstruction in megacolon often results from the enlarged, dysfunctional colon impeding the normal passage of intestinal contents. Differentiating primary from secondary megacolon is critical for treatment, as primary cases may require surgical intervention while secondary causes focus on managing the underlying disease.
Pathophysiology of Intestinal Obstruction
Intestinal obstruction in megacolon results from a failure of normal colonic motility due to neuronal dysfunction or mechanical blockage, leading to impaired passage of intestinal contents. This obstruction causes increased intraluminal pressure, bowel wall distension, and compromised blood flow, which can result in ischemia and necrosis if untreated. The pathophysiology contrasts with simple megacolon, where the primary issue is abnormal colonic dilation without overt obstruction or mechanical blockage.
Clinical Presentation: Megacolon versus Intestinal Obstruction
Megacolon typically presents with progressive abdominal distension, chronic constipation, and abdominal pain due to colonic dilation, whereas intestinal obstruction often manifests with acute onset of severe abdominal pain, vomiting, and absence of bowel movements. In megacolon, symptoms develop gradually over weeks to months alongside signs of colonic inertia, while intestinal obstruction leads to rapid clinical deterioration caused by mechanical blockage. Physical examination in megacolon may reveal a markedly distended abdomen with palpable fecal masses, contrasting with high-pitched bowel sounds and tympany found in intestinal obstruction.
Diagnostic Approaches for Megacolon and Intestinal Obstruction
Diagnostic approaches for Megacolon and Intestinal Obstruction prioritize imaging techniques such as abdominal X-rays, CT scans, and contrast enemas to visualize colonic dilation and identify obstructions. Anorectal manometry and rectal biopsy are essential for distinguishing between congenital causes of Megacolon, like Hirschsprung's disease, and functional obstructions. Laboratory tests and clinical evaluation of symptoms such as abdominal distension, constipation, and pain further guide diagnosis and differentiation between mechanical obstruction and colonic motility disorders.
Key Differences: Megacolon and Intestinal Obstruction
Megacolon refers to an abnormal dilation of the colon often caused by nerve or muscle dysfunction, whereas intestinal obstruction involves a physical blockage that prevents the normal flow of intestinal contents. Megacolon primarily affects colonic motility leading to chronic constipation and distension, while intestinal obstruction can result from causes such as tumors, adhesions, or hernias and typically presents with acute abdominal pain, vomiting, and severe distension. Diagnosis relies on imaging studies like abdominal X-rays and CT scans, with treatment varying from medical management in megacolon to surgical intervention in cases of obstruction.
Complications Associated with Megacolon
Megacolon increases the risk of severe complications such as intestinal obstruction, perforation, and ischemia due to prolonged dilation and impaired motility. Intestinal obstruction caused by megacolon can lead to fecal impaction, necrosis, and toxic megacolon, which requires immediate medical intervention. Chronic megacolon may also cause electrolyte imbalances, bacterial overgrowth, and sepsis, emphasizing the need for timely diagnosis and treatment.
Treatment Modalities: Megacolon vs Intestinal Obstruction
Treatment modalities for megacolon primarily focus on relieving chronic constipation and reducing colonic distention through dietary changes, laxatives, enemas, and in severe cases, surgical intervention such as colectomy. In contrast, intestinal obstruction treatment emphasizes emergency management to restore bowel patency, including nasogastric decompression, intravenous fluids, and often surgical removal of the obstructing lesion or adhesions. Both conditions may require surgery, but megacolon surgery aims to prevent recurrence, while obstruction surgery targets immediate resolution of the blockage.
Prognosis and Long-Term Outcomes
Megacolon with intestinal obstruction presents a higher risk of complications such as perforation, sepsis, and chronic bowel dysfunction, leading to a more guarded prognosis compared to isolated megacolon. Long-term outcomes for megacolon without obstruction often involve manageable symptoms with medical or surgical interventions, whereas cases complicated by obstruction require more intensive treatment and have increased morbidity. Early diagnosis and appropriate management significantly improve survival rates and quality of life in both conditions.
Megacolon and Intestinal Obstruction Infographic
 libterm.com
libterm.com