Chronic kidney disease (CKD) progressively impairs kidney function, leading to waste buildup, fluid imbalance, and complications like high blood pressure and anemia. Early detection and management through lifestyle changes and medication can slow disease progression and improve quality of life. Discover effective strategies to protect your kidneys and manage CKD by reading the rest of this article.
Table of Comparison
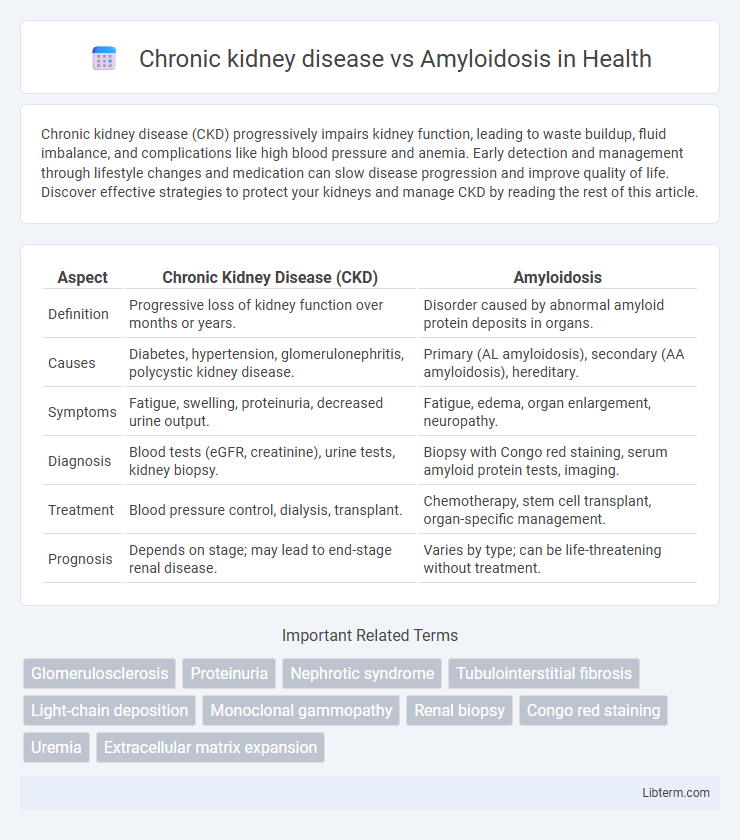
| Aspect | Chronic Kidney Disease (CKD) | Amyloidosis |
|---|---|---|
| Definition | Progressive loss of kidney function over months or years. | Disorder caused by abnormal amyloid protein deposits in organs. |
| Causes | Diabetes, hypertension, glomerulonephritis, polycystic kidney disease. | Primary (AL amyloidosis), secondary (AA amyloidosis), hereditary. |
| Symptoms | Fatigue, swelling, proteinuria, decreased urine output. | Fatigue, edema, organ enlargement, neuropathy. |
| Diagnosis | Blood tests (eGFR, creatinine), urine tests, kidney biopsy. | Biopsy with Congo red staining, serum amyloid protein tests, imaging. |
| Treatment | Blood pressure control, dialysis, transplant. | Chemotherapy, stem cell transplant, organ-specific management. |
| Prognosis | Depends on stage; may lead to end-stage renal disease. | Varies by type; can be life-threatening without treatment. |
Understanding Chronic Kidney Disease
Chronic kidney disease (CKD) is a progressive condition characterized by the gradual loss of kidney function, leading to impaired waste filtration and fluid balance. Differentiating CKD from amyloidosis is crucial, as amyloidosis involves abnormal protein deposits that can cause kidney damage but also affect multiple organs. Early detection and management of CKD through monitoring glomerular filtration rate (GFR) and albuminuria levels are essential to slow disease progression and reduce complications.
What is Amyloidosis?
Amyloidosis is a rare disease characterized by the abnormal accumulation of amyloid proteins in organs and tissues, leading to organ dysfunction. Unlike chronic kidney disease, which primarily involves progressive loss of kidney function, amyloidosis affects multiple systems, including the kidneys, heart, liver, and nervous system. Early diagnosis and treatment are crucial to manage amyloidosis and prevent irreversible organ damage.
Causes of Chronic Kidney Disease
Chronic kidney disease (CKD) primarily results from diabetes mellitus, hypertension, and glomerulonephritis. Amyloidosis, characterized by abnormal protein deposits, can also lead to CKD by damaging renal tissues. Understanding these causes is crucial for early diagnosis and targeted treatment of kidney impairment.
Causes and Types of Amyloidosis
Chronic kidney disease (CKD) primarily results from diabetes, hypertension, and glomerulonephritis, leading to gradual loss of kidney function. Amyloidosis, caused by abnormal protein fibril deposits, includes types such as AL (light-chain), AA (secondary), and hereditary forms, each with distinct protein origins and systemic impacts. The accumulation of amyloid proteins in organs, including kidneys, disrupts normal function, often causing nephrotic syndrome and progressive renal impairment in affected patients.
Symptoms: CKD vs Amyloidosis
Chronic kidney disease (CKD) commonly presents with symptoms such as fatigue, swelling in the legs and ankles, and changes in urine output or color due to impaired kidney function. Amyloidosis often manifests with symptoms like unexplained weight loss, numbness or tingling in the hands and feet, and proteinuria, reflecting amyloid protein deposits disrupting organ function, including the kidneys. Both conditions can cause kidney-related symptoms, but amyloidosis typically includes systemic signs beyond the kidneys, influencing diagnostic differentiation.
Diagnostic Approaches for Both Conditions
Chronic kidney disease (CKD) diagnosis primarily relies on estimating glomerular filtration rate (eGFR) using serum creatinine levels, alongside urine albumin-to-creatinine ratio (ACR) to assess kidney damage. Amyloidosis diagnosis involves a tissue biopsy stained with Congo red to identify amyloid deposits, complemented by serum and urine protein electrophoresis with immunofixation to detect monoclonal light chains. Advanced imaging techniques such as cardiac MRI and SAP scintigraphy support amyloidosis evaluation, whereas CKD staging depends on serial eGFR measurements and renal ultrasound to monitor structural changes.
Treatment Options: Comparative Overview
Chronic kidney disease (CKD) treatment primarily involves managing underlying conditions such as hypertension and diabetes through medications like angiotensin-converting enzyme inhibitors and lifestyle modifications to slow progression. Amyloidosis treatment focuses on reducing amyloid protein production using chemotherapy agents like bortezomib or immunotherapy, with organ-specific interventions including dialysis for kidney involvement. Both diseases may require supportive care including nutritional management and symptom control, but amyloidosis demands targeted plasma cell or genetic therapy, unlike the broader approach in CKD.
Disease Progression and Prognosis
Chronic kidney disease (CKD) typically progresses through stages marked by declining glomerular filtration rate (GFR), leading to end-stage renal disease (ESRD) over years, with prognosis influenced by underlying causes and comorbidities. Amyloidosis involves the deposition of misfolded amyloid proteins in kidney tissues, causing rapid deterioration of renal function and often leading to nephrotic syndrome, with prognosis depending on the amyloid type and treatment response. While CKD progression is generally gradual and monitored via biomarkers like serum creatinine and albuminuria, amyloidosis progression can be more aggressive, frequently requiring early intervention to improve survival outcomes.
Managing Complications in CKD and Amyloidosis
Managing complications in chronic kidney disease (CKD) involves controlling hypertension, electrolyte imbalances, and anemia to slow disease progression and reduce cardiovascular risks. In amyloidosis, treatment focuses on reducing amyloid protein deposition through chemotherapy or targeted therapies, while managing organ dysfunction such as nephrotic syndrome and heart failure. Both conditions require careful monitoring of renal function and tailored interventions to prevent end-stage renal disease and improve patient outcomes.
Prevention and Lifestyle Modifications
Managing Chronic Kidney Disease (CKD) involves strict control of blood pressure, blood sugar, and regular monitoring of kidney function to prevent progression; adopting a low-sodium, kidney-friendly diet and maintaining hydration supports renal health. Amyloidosis prevention centers on early detection and treatment of underlying conditions like multiple myeloma or chronic inflammatory diseases, while a balanced diet and avoiding nephrotoxic substances minimize organ damage risks. Lifestyle modifications for both conditions emphasize smoking cessation, regular exercise, and weight management to reduce systemic inflammation and preserve kidney function.
Chronic kidney disease Infographic
 libterm.com
libterm.com