Thrombocytopenia is a condition characterized by an abnormally low platelet count, which can lead to excessive bleeding and bruising due to impaired blood clotting. Various causes include bone marrow disorders, certain medications, autoimmune diseases, and infections, making accurate diagnosis essential for effective treatment. Discover more about the symptoms, causes, and treatment options for thrombocytopenia in the full article.
Table of Comparison
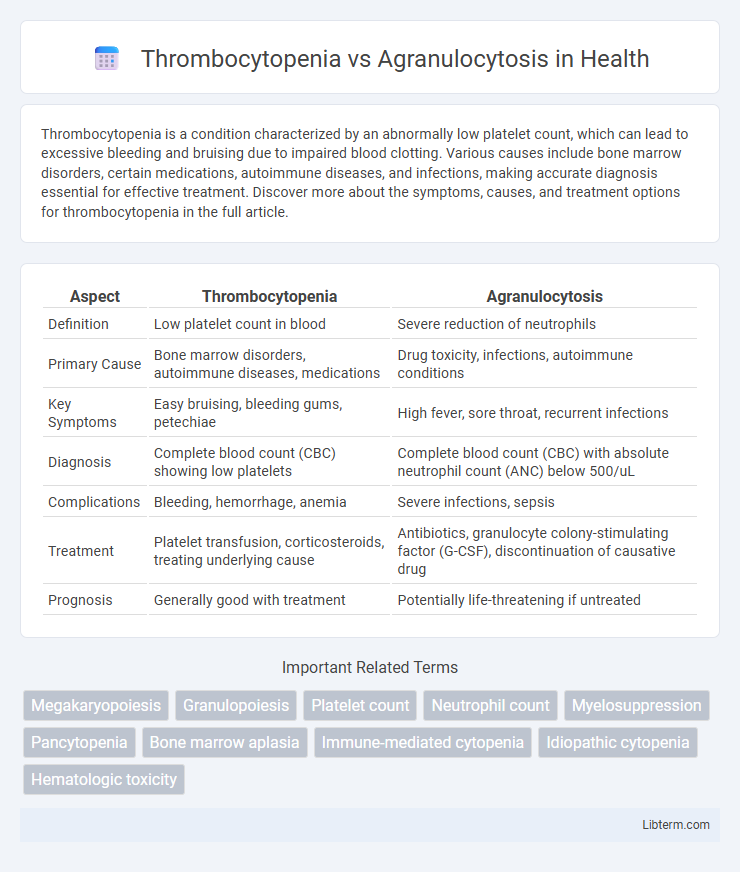
| Aspect | Thrombocytopenia | Agranulocytosis |
|---|---|---|
| Definition | Low platelet count in blood | Severe reduction of neutrophils |
| Primary Cause | Bone marrow disorders, autoimmune diseases, medications | Drug toxicity, infections, autoimmune conditions |
| Key Symptoms | Easy bruising, bleeding gums, petechiae | High fever, sore throat, recurrent infections |
| Diagnosis | Complete blood count (CBC) showing low platelets | Complete blood count (CBC) with absolute neutrophil count (ANC) below 500/uL |
| Complications | Bleeding, hemorrhage, anemia | Severe infections, sepsis |
| Treatment | Platelet transfusion, corticosteroids, treating underlying cause | Antibiotics, granulocyte colony-stimulating factor (G-CSF), discontinuation of causative drug |
| Prognosis | Generally good with treatment | Potentially life-threatening if untreated |
Introduction to Thrombocytopenia and Agranulocytosis
Thrombocytopenia is a hematological disorder characterized by an abnormally low platelet count, increasing the risk of bleeding and bruising. Agranulocytosis, on the other hand, involves a severe reduction in granulocytes, mainly neutrophils, leading to heightened vulnerability to infections. Both conditions are critical blood cell deficiencies but differ in cell type affected and clinical implications.
Definition and Key Differences
Thrombocytopenia is characterized by a reduced platelet count leading to impaired blood clotting, whereas agranulocytosis involves a severe deficiency of granulocytes, particularly neutrophils, resulting in heightened infection risk. The key difference lies in their affected blood components: thrombocytopenia impacts platelets essential for coagulation, while agranulocytosis affects white blood cells critical for immune defense. Diagnosis depends on complete blood count (CBC) analysis, highlighting low platelets in thrombocytopenia and markedly decreased neutrophils in agranulocytosis.
Causes of Thrombocytopenia
Thrombocytopenia primarily results from decreased platelet production due to bone marrow disorders such as leukemia, aplastic anemia, or chemotherapy effects, as well as increased platelet destruction caused by immune thrombocytopenic purpura (ITP), infections, or drug-induced reactions. In contrast, agranulocytosis is characterized by a severe reduction in neutrophil granulocytes, often triggered by adverse drug reactions, autoimmune diseases, or bone marrow suppression. Understanding the distinct hematological profiles and etiologies of thrombocytopenia and agranulocytosis aids in targeted diagnostic and therapeutic approaches.
Causes of Agranulocytosis
Agranulocytosis primarily results from severe bone marrow suppression caused by certain medications such as clozapine, methimazole, and sulfonamides, as well as chemotherapy agents. Autoimmune disorders and infections like viral hepatitis can also trigger agranulocytosis by destroying granulocytes or impairing their production. Unlike thrombocytopenia, which involves low platelet counts, agranulocytosis specifically denotes a critical reduction in neutrophils, leading to increased susceptibility to bacterial and fungal infections.
Pathophysiology: Platelets vs. Granulocytes
Thrombocytopenia involves a decreased platelet count resulting from impaired platelet production, increased destruction, or sequestration, which disrupts hemostasis and increases bleeding risk. Agranulocytosis is characterized by a severe reduction in granulocytes, particularly neutrophils, caused by bone marrow suppression or immune-mediated destruction, compromising the body's ability to fight infections. Both conditions reflect bone marrow dysfunction but differ fundamentally in the affected cell lineage and clinical manifestations related to bleeding versus infection susceptibility.
Clinical Manifestations and Symptoms
Thrombocytopenia primarily presents with symptoms such as easy bruising, petechiae, prolonged bleeding from cuts, and mucosal bleeding due to low platelet counts affecting clot formation. Agranulocytosis is characterized by severe neutropenia leading to recurrent infections, fever, sore throat, and ulcerations in the oral cavity as the body's immune defense is compromised. Both conditions require prompt clinical evaluation to prevent complications related to bleeding and infections respectively.
Diagnostic Approaches
Thrombocytopenia is diagnosed primarily through a complete blood count (CBC) showing a low platelet count, often supplemented by peripheral blood smear and bone marrow biopsy to identify underlying causes. Agranulocytosis diagnosis involves a CBC revealing severe neutropenia, typically confirmed by bone marrow examination to assess granulocyte precursor status. Both conditions may require further immunological and infectious disease testing to clarify etiology and guide treatment.
Treatment Strategies
Thrombocytopenia treatment centers on platelet transfusions, corticosteroids, and addressing underlying causes such as immune disorders or infections, while severe cases may require splenectomy or thrombopoietin receptor agonists like eltrombopag. Agranulocytosis demands immediate antibiotic therapy to counteract severe neutropenia-related infections, with granulocyte colony-stimulating factor (G-CSF) being a critical agent to promote neutrophil recovery. Managing both conditions involves close hematologic monitoring, supportive care, and tailored interventions based on etiology and severity.
Complications and Prognosis
Thrombocytopenia, characterized by a low platelet count, primarily increases the risk of bleeding complications, such as petechiae, mucosal hemorrhages, and severe intracranial hemorrhage, potentially leading to life-threatening situations if untreated. Agranulocytosis, defined by an extremely low neutrophil count, heightens vulnerability to severe infections, sepsis, and septic shock due to impaired immune response, with prognosis heavily dependent on prompt antibiotic treatment and bone marrow recovery. Both conditions require early diagnosis and intervention to improve patient outcomes, with prognosis varying based on severity, underlying cause, and timely management.
Prevention and Monitoring Tips
Prevent thrombocytopenia by avoiding medications linked to platelet reduction and managing underlying conditions such as liver disease or infections, while regular platelet count monitoring helps detect early declines. For agranulocytosis, minimize risk by careful use of drugs like clozapine or antithyroid agents, with frequent complete blood count (CBC) testing to monitor neutrophil levels and prompt identification of infections. Consistent clinical evaluation and patient education on symptoms like unexplained bruising or persistent fever enhance early intervention and improve outcomes for both conditions.
Thrombocytopenia Infographic
 libterm.com
libterm.com