Hyperglycemia occurs when blood sugar levels rise above normal, often linked to diabetes and inadequate insulin function. Persistent hyperglycemia can lead to serious complications such as nerve damage, kidney disease, and cardiovascular issues. Discover how to recognize signs, manage your symptoms effectively, and prevent long-term health risks in the rest of this article.
Table of Comparison
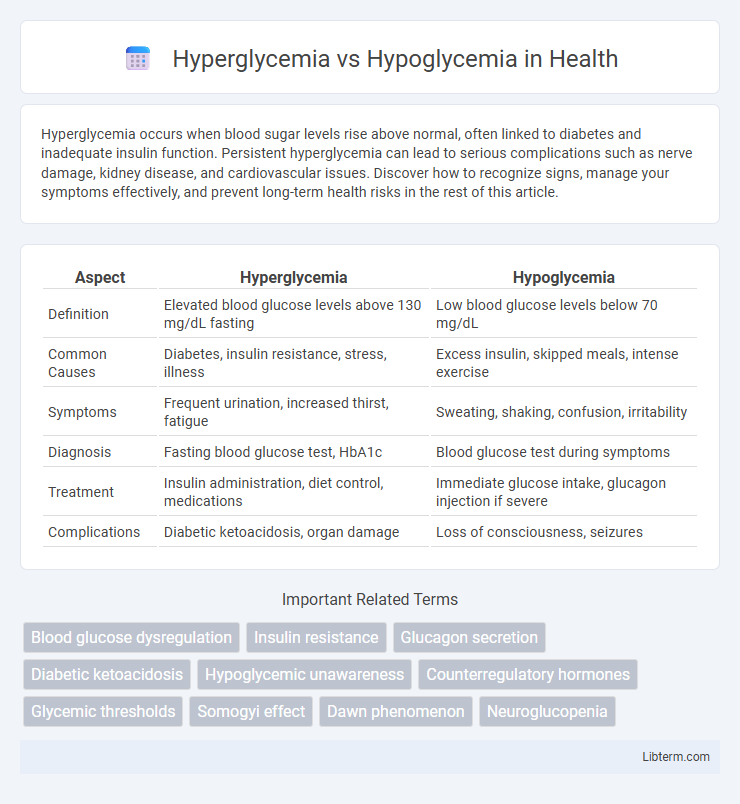
| Aspect | Hyperglycemia | Hypoglycemia |
|---|---|---|
| Definition | Elevated blood glucose levels above 130 mg/dL fasting | Low blood glucose levels below 70 mg/dL |
| Common Causes | Diabetes, insulin resistance, stress, illness | Excess insulin, skipped meals, intense exercise |
| Symptoms | Frequent urination, increased thirst, fatigue | Sweating, shaking, confusion, irritability |
| Diagnosis | Fasting blood glucose test, HbA1c | Blood glucose test during symptoms |
| Treatment | Insulin administration, diet control, medications | Immediate glucose intake, glucagon injection if severe |
| Complications | Diabetic ketoacidosis, organ damage | Loss of consciousness, seizures |
Understanding Blood Glucose: Hyperglycemia vs Hypoglycemia
Hyperglycemia refers to elevated blood glucose levels typically above 130 mg/dL fasting, often linked to diabetes, causing symptoms like frequent urination, increased thirst, and fatigue. Hypoglycemia occurs when blood glucose drops below 70 mg/dL, leading to shakiness, confusion, sweating, and potential loss of consciousness. Monitoring blood sugar is crucial for managing these conditions, as maintaining glucose within the target range of 70-130 mg/dL fasting prevents complications and supports overall metabolic health.
Key Differences Between Hyperglycemia and Hypoglycemia
Hyperglycemia is characterized by elevated blood glucose levels typically above 130 mg/dL fasting or 180 mg/dL postprandial, whereas hypoglycemia involves abnormally low blood glucose levels, usually below 70 mg/dL. Symptoms of hyperglycemia include frequent urination, increased thirst, and blurred vision, in contrast to hypoglycemia which presents with shakiness, sweating, confusion, and potential loss of consciousness. Management of hyperglycemia often requires insulin or oral hypoglycemic agents, while hypoglycemia is treated with quick-absorbing carbohydrates like glucose tablets or juice to rapidly raise blood sugar levels.
Common Causes of High and Low Blood Sugar
Hyperglycemia commonly results from insufficient insulin production, stress, illness, or excessive consumption of carbohydrates and sugary foods, leading to elevated blood glucose levels often seen in diabetes. Hypoglycemia typically arises from excessive insulin administration, prolonged fasting, intense physical activity, or certain medications, causing dangerously low blood sugar levels. Both conditions require careful monitoring of blood glucose and lifestyle adjustments to maintain optimal metabolic balance.
Recognizing Symptoms: Hyperglycemia vs Hypoglycemia
Hyperglycemia symptoms include frequent urination, increased thirst, and blurred vision, while hypoglycemia presents with sweating, shakiness, and confusion. Recognizing these distinct signs is crucial for timely intervention and preventing complications. Continuous glucose monitoring devices aid in real-time detection, enhancing management of blood sugar fluctuations.
Risk Factors: Who Is Most Susceptible?
Individuals with diabetes are most susceptible to both hyperglycemia and hypoglycemia due to impaired insulin regulation. Risk factors for hyperglycemia include poor management of diabetes, illness, stress, and certain medications, while hypoglycemia is often triggered by excessive insulin, skipping meals, or intense physical activity. Elderly patients, children with type 1 diabetes, and those with irregular eating habits or medical conditions affecting glucose metabolism face heightened vulnerability to these blood sugar imbalances.
Short-term and Long-term Health Consequences
Hyperglycemia causes short-term symptoms like frequent urination, increased thirst, and fatigue, while long-term consequences include nerve damage, kidney disease, and cardiovascular complications. Hypoglycemia triggers immediate effects such as sweating, shakiness, confusion, and in severe cases, seizures or loss of consciousness, with repeated episodes potentially leading to cognitive impairment over time. Both conditions require careful management to prevent acute complications and reduce the risk of chronic health issues.
Diagnosis: How Are Blood Sugar Imbalances Detected?
Blood sugar imbalances are detected through blood glucose tests such as fasting plasma glucose (FPG), oral glucose tolerance test (OGTT), and glycated hemoglobin (HbA1c) levels. Hyperglycemia is diagnosed when fasting blood glucose exceeds 126 mg/dL or HbA1c levels are above 6.5%. Hypoglycemia is identified when blood glucose levels fall below 70 mg/dL, often confirmed by self-monitoring of blood glucose or continuous glucose monitoring systems.
Immediate and Long-term Treatment Options
Immediate treatment of hyperglycemia involves administering insulin or oral hypoglycemic agents to rapidly reduce elevated blood glucose levels, while severe cases may require intravenous fluids and electrolyte replacement to prevent diabetic ketoacidosis. Immediate management of hypoglycemia includes fast-acting glucose sources such as oral glucose tablets, fruit juice, or intravenous dextrose to quickly restore normal blood sugar levels and prevent neurological damage. Long-term treatment for hyperglycemia focuses on lifestyle modifications, consistent blood glucose monitoring, and medication adherence to maintain glycemic control and prevent complications, whereas hypoglycemia prevention involves adjusting antidiabetic medications and dietary planning to avoid recurrent low blood sugar episodes.
Prevention Strategies for Managing Blood Sugar
Effective prevention strategies for managing blood sugar focus on maintaining balanced glucose levels to avoid hyperglycemia and hypoglycemia. For hyperglycemia, key measures include consistent carbohydrate monitoring, regular physical activity, and appropriate insulin management, while hypoglycemia prevention emphasizes timely meals, tailored medication dosages, and frequent blood sugar testing. Implementing personalized diabetes care plans with guidance from healthcare professionals ensures optimal glucose control and reduces the risk of acute complications.
When to Seek Medical Attention
Seek medical attention for hyperglycemia when blood glucose levels exceed 250 mg/dL persistently, accompanied by symptoms such as excessive thirst, frequent urination, or confusion, as this may indicate diabetic ketoacidosis requiring urgent care. In cases of hypoglycemia, immediate medical intervention is necessary if blood sugar drops below 70 mg/dL with symptoms like sweating, trembling, irritability, or loss of consciousness, to prevent severe complications such as seizures. Timely recognition and treatment of these critical glucose abnormalities are essential for avoiding long-term damage or life-threatening emergencies.
Hyperglycemia Infographic
 libterm.com
libterm.com