Leukopenia is a condition characterized by a significantly reduced number of white blood cells, weakening your immune system's ability to fight infections. Causes range from bone marrow disorders and autoimmune diseases to certain medications and viral infections. Explore the full article to understand symptoms, diagnosis, and treatment options for leukopenia.
Table of Comparison
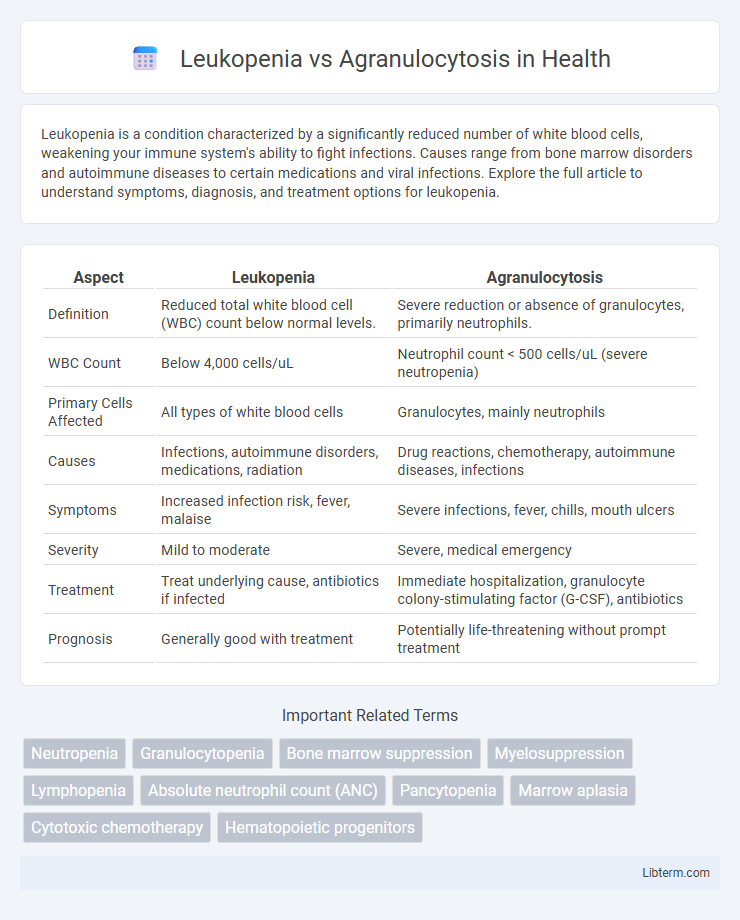
| Aspect | Leukopenia | Agranulocytosis |
|---|---|---|
| Definition | Reduced total white blood cell (WBC) count below normal levels. | Severe reduction or absence of granulocytes, primarily neutrophils. |
| WBC Count | Below 4,000 cells/uL | Neutrophil count < 500 cells/uL (severe neutropenia) |
| Primary Cells Affected | All types of white blood cells | Granulocytes, mainly neutrophils |
| Causes | Infections, autoimmune disorders, medications, radiation | Drug reactions, chemotherapy, autoimmune diseases, infections |
| Symptoms | Increased infection risk, fever, malaise | Severe infections, fever, chills, mouth ulcers |
| Severity | Mild to moderate | Severe, medical emergency |
| Treatment | Treat underlying cause, antibiotics if infected | Immediate hospitalization, granulocyte colony-stimulating factor (G-CSF), antibiotics |
| Prognosis | Generally good with treatment | Potentially life-threatening without prompt treatment |
Introduction to Leukopenia and Agranulocytosis
Leukopenia is a medical condition characterized by a reduced white blood cell count, impairing the body's ability to fight infections. Agranulocytosis is a severe form of leukopenia marked by an extremely low number of granulocytes, particularly neutrophils, increasing the risk of serious infections. Both conditions require prompt diagnosis and treatment to prevent complications related to immune system deficiency.
Definition: Leukopenia
Leukopenia is a medical condition characterized by a reduced white blood cell count, primarily affecting neutrophils, which weakens the immune system. Agranulocytosis represents a severe form of leukopenia marked by an extremely low number of granulocytes, especially neutrophils, leading to a heightened risk of infections. Understanding leukopenia's impact on immune function aids in distinguishing it from the more critical agranulocytosis.
Definition: Agranulocytosis
Agranulocytosis is a severe form of leukopenia characterized by an extremely low count of granulocytes, particularly neutrophils, leading to a critical weakening of the immune system. This condition significantly increases the risk of infections and is often drug-induced or a result of bone marrow failure. Unlike general leukopenia, agranulocytosis involves near-total depletion of granulocytes, making it a medical emergency requiring immediate intervention.
Key Differences Between Leukopenia and Agranulocytosis
Leukopenia refers to a general decrease in white blood cell count, while agranulocytosis specifically denotes a severe reduction in granulocytes, particularly neutrophils. Leukopenia can involve various types of white cells, making it a broader condition, whereas agranulocytosis primarily impairs the body's ability to fight bacterial infections due to neutrophil deficiency. The severity and clinical implications differ as agranulocytosis presents a higher risk for severe infections and requires more urgent medical intervention compared to leukopenia.
Causes of Leukopenia
Leukopenia is primarily caused by bone marrow suppression due to infections, autoimmune diseases, or chemotherapy, which leads to a decreased production of white blood cells. Agranulocytosis is a severe form of leukopenia characterized by an extreme reduction in neutrophils, often triggered by drug reactions, such as antithyroid medications or clozapine. Understanding these causes is critical for diagnosis and targeted treatment in hematologic disorders.
Causes of Agranulocytosis
Agranulocytosis is primarily caused by severe drug-induced bone marrow suppression, with common culprits including antithyroid medications, chemotherapy agents, and certain antibiotics like penicillin. Autoimmune disorders and viral infections such as HIV and hepatitis also contribute to the development of agranulocytosis by impairing granulocyte production. Unlike leukopenia, which refers to a general reduction in white blood cells, agranulocytosis specifically denotes an almost complete absence of granulocytes, making it a more severe and life-threatening condition.
Common Symptoms and Clinical Manifestations
Leukopenia presents with frequent infections, fever, and fatigue due to a decreased white blood cell count, especially neutrophils. Agranulocytosis, a severe form of leukopenia, manifests with sudden high fever, chills, sore throat, and mouth ulcers, indicating a critical drop in granulocytes. Both conditions require urgent medical evaluation to prevent potentially life-threatening infections and complications.
Diagnostic Criteria and Laboratory Findings
Leukopenia is characterized by a white blood cell count below 4,000 cells/uL, while agranulocytosis involves a severe reduction in granulocytes, particularly neutrophils, often below 500 cells/uL. Diagnostic criteria for leukopenia involve a complete blood count (CBC) revealing decreased total leukocytes, whereas agranulocytosis diagnosis relies on a CBC showing extreme neutropenia and bone marrow biopsy indicating granulocytic aplasia. Laboratory findings in leukopenia may show a proportional reduction across leukocyte types, but agranulocytosis distinctly manifests with profound neutropenia and increased susceptibility to infections.
Treatment Approaches and Management Strategies
Leukopenia treatment focuses on addressing underlying causes such as infections, autoimmune diseases, or drug-induced suppression, with supportive therapies including antibiotics and growth factors like granulocyte colony-stimulating factor (G-CSF). Agranulocytosis management requires immediate cessation of offending agents, aggressive infection control, and often hospitalization for intravenous antibiotics and G-CSF to rapidly restore neutrophil counts. Both conditions necessitate regular blood count monitoring and individualized treatment plans to prevent severe infections and complications.
Prognosis and Prevention Tips
Leukopenia prognosis varies widely depending on its underlying cause, with mild cases often resolving with treatment, while severe leukopenia increases infection risk and requires careful monitoring. Agranulocytosis carries a more severe prognosis due to a critical drop in neutrophils, leading to life-threatening infections and requiring immediate medical intervention. Prevention tips for both conditions include avoiding exposure to known bone marrow toxins, regular blood count monitoring during high-risk medication use, and maintaining good hygiene to reduce infection risk.
Leukopenia Infographic
 libterm.com
libterm.com