Urolithiasis causes kidney stones that can block urinary flow, leading to intense pain and possible urinary tract infections like pyelonephritis. Pyelonephritis is a bacterial infection of the kidney that can cause fever, flank pain, and potentially serious complications if untreated. Discover more about how these conditions are related and effective treatment options to protect your kidney health.
Table of Comparison
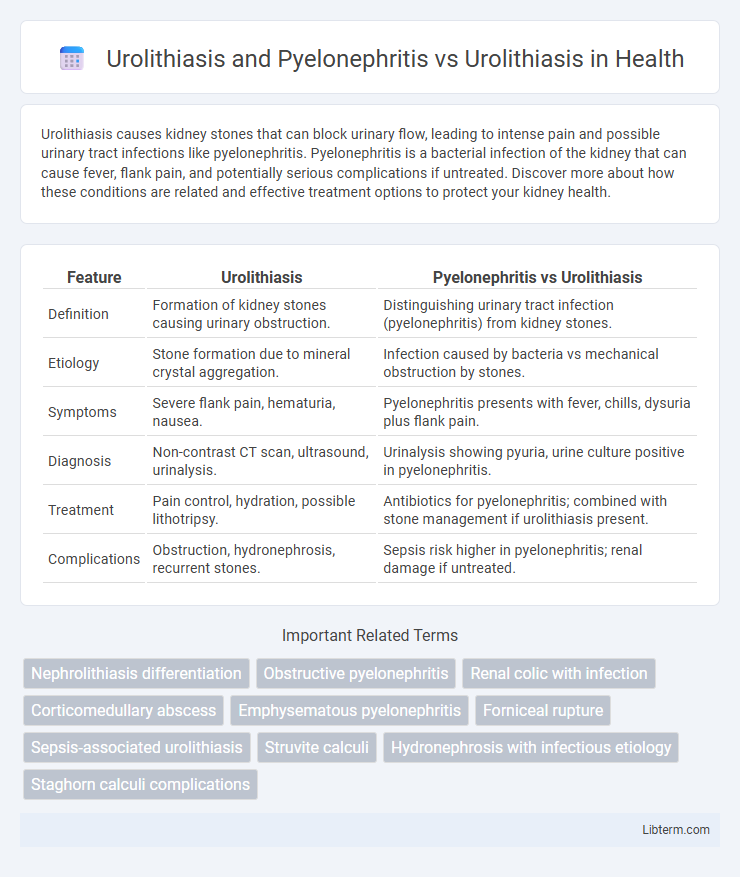
| Feature | Urolithiasis | Pyelonephritis vs Urolithiasis |
|---|---|---|
| Definition | Formation of kidney stones causing urinary obstruction. | Distinguishing urinary tract infection (pyelonephritis) from kidney stones. |
| Etiology | Stone formation due to mineral crystal aggregation. | Infection caused by bacteria vs mechanical obstruction by stones. |
| Symptoms | Severe flank pain, hematuria, nausea. | Pyelonephritis presents with fever, chills, dysuria plus flank pain. |
| Diagnosis | Non-contrast CT scan, ultrasound, urinalysis. | Urinalysis showing pyuria, urine culture positive in pyelonephritis. |
| Treatment | Pain control, hydration, possible lithotripsy. | Antibiotics for pyelonephritis; combined with stone management if urolithiasis present. |
| Complications | Obstruction, hydronephrosis, recurrent stones. | Sepsis risk higher in pyelonephritis; renal damage if untreated. |
Overview of Urolithiasis
Urolithiasis refers to the formation of stones in the urinary tract, primarily in the kidneys, caused by supersaturation of urine with minerals such as calcium, oxalate, and uric acid. These stones can lead to obstruction, pain, hematuria, and increased risk of infections like pyelonephritis, an inflammation of the kidney due to bacterial infection. Effective diagnosis includes imaging techniques like CT scans and urinalysis, while treatment ranges from conservative management to surgical intervention depending on stone size and location.
Pathophysiology of Urolithiasis
Urolithiasis involves the formation of crystalline stones within the urinary tract due to supersaturation of urine with stone-forming solutes such as calcium, oxalate, and uric acid. Pyelonephritis in the context of urolithiasis occurs when obstructive calculi impair urinary flow, leading to bacterial infection and inflammation of the renal pelvis and parenchyma. The pathophysiology of urolithiasis centers on stone nucleation, crystal growth, and aggregation facilitated by urinary stasis and altered pH, which increase the risk for recurrent stone formation and secondary infections like pyelonephritis.
Clinical Presentation of Urolithiasis
Urolithiasis typically presents with sudden onset of severe flank pain radiating to the groin, hematuria, nausea, and vomiting due to obstruction of the urinary tract by calculi. In contrast, pyelonephritis accompanied by urolithiasis shows systemic symptoms including fever, chills, and dysuria along with localized tenderness in the costovertebral angle. Clinical evaluation of urolithiasis relies heavily on recognizing acute renal colic and hematuria, whereas pyelonephritis requires assessment for signs of infection and systemic inflammation.
What is Pyelonephritis?
Pyelonephritis is a severe kidney infection that occurs when bacteria ascend from the lower urinary tract, often complicating Urolithiasis cases. Urolithiasis involves the formation of kidney stones, which can obstruct urine flow and increase the risk of bacterial infection leading to pyelonephritis. Managing pyelonephritis alongside urolithiasis requires prompt antibiotic therapy and sometimes surgical intervention to remove obstructive stones.
Pathophysiology of Pyelonephritis in Urolithiasis
Urolithiasis causes urinary tract obstruction that impairs urine flow and promotes stasis, creating an environment conducive to bacterial colonization and ascending infection leading to pyelonephritis. The obstruction increases intrarenal pressure, compromising renal tissue perfusion and facilitating bacterial invasion from the lower urinary tract to the renal parenchyma. This pathophysiological process exacerbates inflammatory responses, resulting in renal scarring and potential loss of kidney function if untreated.
Distinguishing Urolithiasis Alone vs. Urolithiasis with Pyelonephritis
Urolithiasis presents primarily with renal colic, hematuria, and localized flank pain caused by urinary tract stones obstructing urine flow, whereas Urolithiasis with pyelonephritis manifests additional systemic symptoms including fever, chills, and flank tenderness due to renal parenchymal infection. Diagnostic imaging such as non-contrast CT scans reveals urinary calculi in both conditions, but the presence of inflammatory changes, renal enlargement, and perinephric stranding on CT favors pyelonephritis. Laboratory findings in Urolithiasis alone typically show hematuria and normal or mildly elevated inflammatory markers, while combined pyelonephritis is marked by leukocytosis, positive urine cultures, and elevated inflammatory markers like C-reactive protein.
Diagnostic Approaches for Both Conditions
Diagnostic approaches for urolithiasis primarily involve imaging techniques such as non-contrast helical CT scans, which provide detailed detection of urinary stones, and ultrasound for initial assessment, especially in pregnant patients. In pyelonephritis, diagnosis is confirmed through clinical evaluation of symptoms like flank pain and fever, supported by urinalysis showing pyuria and bacteriuria, along with imaging such as ultrasound or contrast-enhanced CT to detect renal inflammation or abscess. Combining imaging and laboratory tests is essential in differentiating uncomplicated urolithiasis from pyelonephritis, ensuring targeted treatment through accurate diagnosis.
Management Strategies: Urolithiasis vs. Urolithiasis with Pyelonephritis
Management of urolithiasis with pyelonephritis requires prompt antibiotic therapy targeting common pathogens like Escherichia coli and ureteral decompression via stenting or nephrostomy to prevent sepsis. In contrast, uncomplicated urolithiasis focuses on analgesia, hydration, and medical expulsive therapy using alpha-blockers to facilitate stone passage. Imaging modalities such as CT urography guide intervention decisions, with invasive procedures reserved for persistent obstruction or infection complications.
Prognosis and Complications
Urolithiasis combined with pyelonephritis presents a more severe prognosis due to the risk of ascending urinary tract infections leading to renal parenchymal damage, sepsis, or abscess formation, compared to isolated urolithiasis which primarily causes obstruction and renal colic. Complications in urolithiasis with pyelonephritis include chronic kidney disease, recurrent infections, and potential post-obstructive renal failure, whereas uncomplicated urolithiasis mainly risks hydronephrosis and stone migration. Early diagnosis and management of pyelonephritis in patients with urolithiasis are critical to prevent long-term renal impairment and improve clinical outcomes.
Preventive Measures and Patient Education
Preventive measures for Urolithiasis and Pyelonephritis emphasize adequate hydration, dietary modifications to reduce stone formation risk, and timely treatment of urinary tract infections to prevent kidney involvement. Patient education focuses on recognizing early symptoms such as flank pain and fever, adhering to prescribed antibiotic regimens, and maintaining proper hygiene to reduce infection recurrence. Implementing lifestyle changes and regular follow-up imaging can significantly decrease complications associated with both conditions.
Urolithiasis and Pyelonephritis Infographic
 libterm.com
libterm.com