Choledocholithiasis occurs when gallstones block the common bile duct, causing severe abdominal pain, jaundice, and potential complications such as infection or pancreatitis. Timely diagnosis through imaging and appropriate treatment are crucial to prevent serious health risks. Explore the full article to understand the symptoms, diagnosis, and effective management strategies for your care.
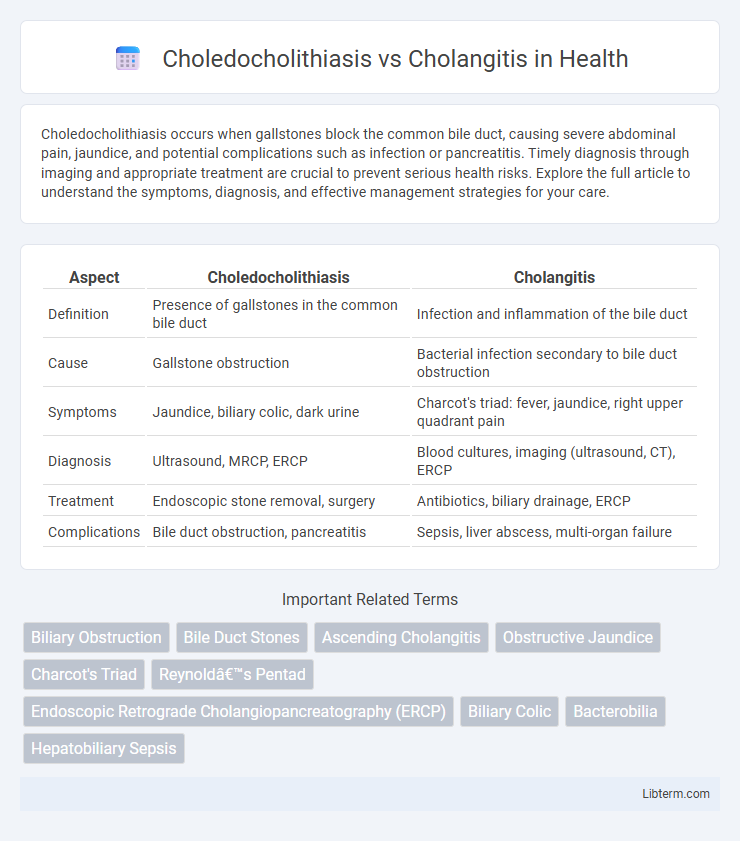
Table of Comparison
| Aspect | Choledocholithiasis | Cholangitis |
|---|---|---|
| Definition | Presence of gallstones in the common bile duct | Infection and inflammation of the bile duct |
| Cause | Gallstone obstruction | Bacterial infection secondary to bile duct obstruction |
| Symptoms | Jaundice, biliary colic, dark urine | Charcot's triad: fever, jaundice, right upper quadrant pain |
| Diagnosis | Ultrasound, MRCP, ERCP | Blood cultures, imaging (ultrasound, CT), ERCP |
| Treatment | Endoscopic stone removal, surgery | Antibiotics, biliary drainage, ERCP |
| Complications | Bile duct obstruction, pancreatitis | Sepsis, liver abscess, multi-organ failure |
Introduction to Choledocholithiasis and Cholangitis
Choledocholithiasis is the presence of gallstones in the common bile duct, often causing biliary obstruction and leading to jaundice or pancreatitis. Cholangitis is an infection of the bile ducts, typically resulting from bile duct obstruction by stones, bacteria, or strictures, and presents with Charcot's triad of fever, jaundice, and right upper quadrant pain. Both conditions are critical biliary disorders requiring prompt diagnosis using imaging modalities such as ultrasound, ERCP, or MRCP for timely management and prevention of complications.
Definition and Clinical Significance
Choledocholithiasis refers to the presence of gallstones in the common bile duct, causing biliary obstruction and potential complications such as jaundice and pancreatitis. Cholangitis is an infection of the bile ducts, often resulting from the obstruction caused by choledocholithiasis, leading to fever, abdominal pain, and sepsis. Understanding these conditions is crucial for timely diagnosis and treatment to prevent severe complications like biliary cirrhosis and systemic infection.
Etiology and Pathogenesis
Choledocholithiasis results from the migration of gallstones from the gallbladder into the common bile duct, causing biliary obstruction and increased ductal pressure. Cholangitis typically arises from bacterial infection superimposed on this obstruction, leading to inflammation and potential biliary sepsis. The pathogenesis of cholangitis involves bile stasis and ascending infection by enteric bacteria such as Escherichia coli, Klebsiella, and Enterococcus species.
Epidemiology and Risk Factors
Choledocholithiasis primarily affects adults over 40, with a higher prevalence in females and individuals with a history of gallstones, obesity, or rapid weight loss. Cholangitis, often secondary to choledocholithiasis, shows increased incidence in patients with biliary obstruction, bile duct strictures, or immunocompromised states. Both conditions are more common in populations with metabolic syndrome, chronic liver disease, and those undergoing biliary procedures.
Clinical Presentation and Symptoms
Choledocholithiasis typically presents with intermittent right upper quadrant abdominal pain, jaundice, and possible dark urine due to bile duct obstruction by gallstones. Cholangitis manifests with Charcot's triad of fever, right upper quadrant pain, and jaundice, often progressing to Reynolds' pentad with hypotension and mental confusion indicating severe infection. Early recognition of cholangitis symptoms is critical due to its potential for rapid systemic sepsis compared to the usually less acute presentation of choledocholithiasis.
Diagnostic Criteria and Imaging Modalities
Choledocholithiasis is identified by the presence of gallstones in the common bile duct, diagnosed through elevated liver enzymes, bilirubin, and imaging modalities like Magnetic Resonance Cholangiopancreatography (MRCP) or Endoscopic Ultrasound (EUS) showing ductal stones. Cholangitis diagnosis involves clinical signs of infection such as fever, jaundice, and right upper quadrant pain (Charcot's triad), with imaging via ultrasound revealing bile duct dilation and potential stones, supplemented by MRCP or Endoscopic Retrograde Cholangiopancreatography (ERCP) for confirmation and therapeutic intervention. Laboratory markers for cholangitis include leukocytosis and elevated inflammatory markers, helping differentiate it from isolated choledocholithiasis.
Laboratory Findings and Biomarker Differences
Choledocholithiasis primarily presents with elevated alkaline phosphatase (ALP) and gamma-glutamyl transferase (GGT) due to bile duct obstruction, whereas cholangitis is characterized by marked leukocytosis, elevated C-reactive protein (CRP), and increased procalcitonin reflecting systemic infection. Liver function tests in cholangitis show significant elevation in bilirubin and transaminases alongside ALP and GGT, indicating both biliary obstruction and inflammation. Blood cultures may be positive in cholangitis, helping distinguish it from choledocholithiasis, which typically lacks systemic infection markers.
Complications and Prognosis
Choledocholithiasis often leads to biliary obstruction, increasing the risk of pancreatitis and recurrent cholangitis, with prognosis heavily dependent on timely stone removal. Cholangitis results in systemic infection and sepsis, presenting a higher risk of severe complications like septic shock and multi-organ failure, demanding urgent antibiotic therapy and biliary decompression for improved outcomes. Both conditions can cause significant morbidity, but untreated or delayed management of cholangitis carries a more acute threat to patient survival.
Management and Treatment Approaches
Management of choledocholithiasis involves endoscopic retrograde cholangiopancreatography (ERCP) for stone extraction and biliary decompression, with laparoscopic cholecystectomy recommended to prevent recurrence. In cholangitis, urgent antibiotic therapy targeting gram-negative and anaerobic bacteria is critical, alongside immediate biliary drainage via ERCP or percutaneous approaches to relieve obstruction. Supportive care includes fluid resuscitation and monitoring for sepsis-related complications to reduce morbidity and mortality.
Prevention Strategies and Follow-Up Recommendations
Preventing choledocholithiasis involves maintaining a healthy diet rich in fiber and low in cholesterol to reduce gallstone formation, along with regular monitoring in patients with a history of gallstones or biliary sludge. Cholangitis prevention emphasizes prompt treatment of biliary obstruction through endoscopic retrograde cholangiopancreatography (ERCP) or surgery to minimize infection risk. Follow-up for choledocholithiasis requires periodic imaging and liver function tests, while cholangitis management includes close clinical monitoring and prophylactic antibiotics in high-risk cases to prevent recurrence.
Choledocholithiasis Infographic
 libterm.com
libterm.com