Nerve block is a medical procedure that involves injecting medication near specific nerves to reduce pain or inflammation. This targeted approach can provide relief from chronic pain, aid in surgical procedures, or diagnose nerve-related conditions. Discover how nerve blocks could improve your treatment options by reading the rest of the article.
Table of Comparison
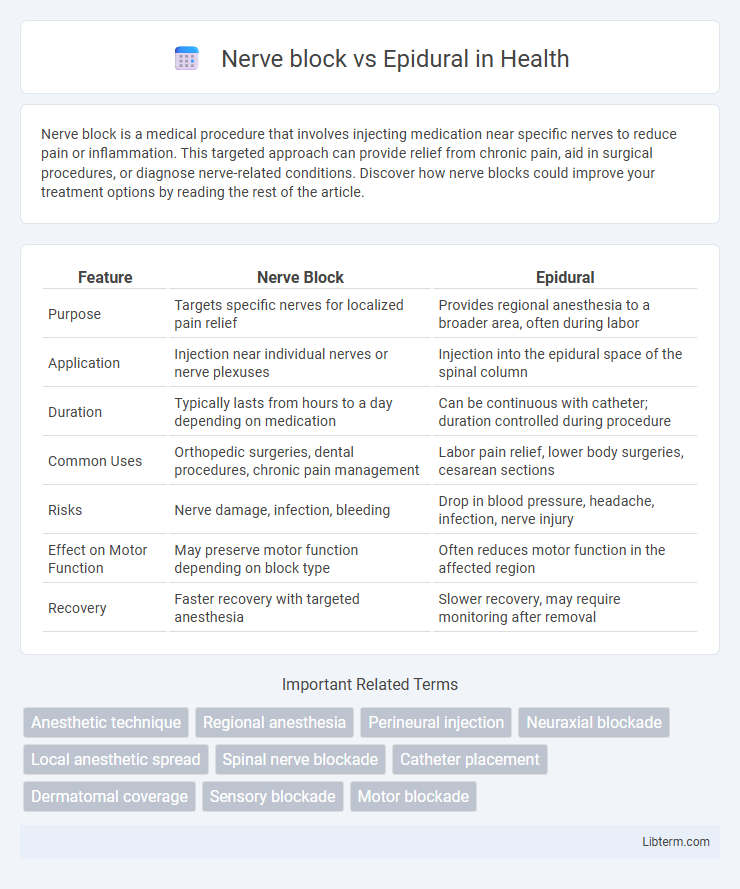
| Feature | Nerve Block | Epidural |
|---|---|---|
| Purpose | Targets specific nerves for localized pain relief | Provides regional anesthesia to a broader area, often during labor |
| Application | Injection near individual nerves or nerve plexuses | Injection into the epidural space of the spinal column |
| Duration | Typically lasts from hours to a day depending on medication | Can be continuous with catheter; duration controlled during procedure |
| Common Uses | Orthopedic surgeries, dental procedures, chronic pain management | Labor pain relief, lower body surgeries, cesarean sections |
| Risks | Nerve damage, infection, bleeding | Drop in blood pressure, headache, infection, nerve injury |
| Effect on Motor Function | May preserve motor function depending on block type | Often reduces motor function in the affected region |
| Recovery | Faster recovery with targeted anesthesia | Slower recovery, may require monitoring after removal |
Introduction to Nerve Blocks and Epidurals
Nerve blocks and epidurals are regional anesthesia techniques used to manage pain during surgical procedures or childbirth by targeting specific nerves or nerve regions. A nerve block involves the injection of anesthetic near a particular nerve or group of nerves to interrupt pain signals, providing localized pain relief. Epidurals consist of injecting anesthetic into the epidural space surrounding the spinal cord, offering broader pain control, commonly utilized in labor and lower body surgeries.
What is a Nerve Block?
A nerve block is a medical procedure that involves injecting anesthetic near specific nerves to interrupt pain signals from a targeted area of the body. It provides localized pain relief during surgeries or for chronic pain management without affecting overall consciousness. Unlike epidurals, which deliver anesthesia into the epidural space around the spinal cord, nerve blocks focus on isolated nerve pathways for precise pain control.
What is an Epidural?
An epidural is a regional anesthesia technique involving the injection of anesthetic agents into the epidural space surrounding the spinal cord to block pain signals from specific areas of the body, commonly used during labor and surgeries. Unlike a nerve block that targets individual nerves or nerve clusters, an epidural affects a broader region by numbing multiple nerve roots at the spinal level. This method provides continuous pain relief through a catheter, allowing adjustable dosing and prolonged anesthesia.
Key Differences Between Nerve Block and Epidural
Nerve blocks target specific nerves or nerve groups to provide localized anesthesia or pain relief, while epidurals deliver medication into the epidural space of the spine, affecting a broader area. Epidurals are commonly used for labor pain or major surgeries requiring extensive numbness, whereas nerve blocks are preferred for certain localized procedures or chronic pain management. The onset of anesthesia in nerve blocks is typically faster and more focused compared to the more gradual and widespread effect of epidurals.
Indications: When to Choose Nerve Block or Epidural
Nerve blocks are typically indicated for targeted pain relief in outpatient procedures or when localized anesthesia is preferred, such as in joint surgeries or minor limb operations. Epidurals are chosen for extensive pain control during labor, cesarean sections, or major abdominal and pelvic surgeries requiring continuous analgesia. Selecting between nerve block and epidural depends on the surgical site, duration of pain relief needed, and the patient's overall medical condition.
Procedure Steps: Nerve Block vs. Epidural
Nerve block procedures involve injecting anesthetic near specific nerves or nerve clusters to target localized pain relief, typically guided by ultrasound or fluoroscopy for precision. Epidural procedures require inserting a catheter into the epidural space of the spinal column to deliver continuous or intermittent pain medication, often used during childbirth or major surgeries. Both techniques demand strict aseptic protocols and careful monitoring to minimize risks such as infection or nerve damage.
Benefits of Nerve Blocks
Nerve blocks offer targeted pain relief by directly interrupting pain signals at specific nerves, resulting in effective and localized analgesia with minimal systemic side effects. They reduce the need for opioid medications, thereby lowering associated risks such as nausea, sedation, and respiratory depression. Nerve blocks also facilitate faster recovery and increased patient mobility compared to epidural anesthesia.
Benefits of Epidural Anesthesia
Epidural anesthesia offers significant benefits such as prolonged pain relief during labor and surgical procedures by delivering continuous medication near the spinal nerves. It allows for adjustable pain control with minimal motor impairment, enabling patients to remain alert and participate actively in childbirth. The technique reduces systemic opioid use and associated side effects, promoting faster recovery and improved maternal comfort.
Risks and Side Effects Comparison
Nerve blocks carry risks such as nerve damage, infection, and localized numbness or weakness, while epidurals pose potential side effects including low blood pressure, severe headache, and spinal cord complications. Both procedures may cause allergic reactions and bleeding, but epidurals often warrant closer monitoring due to the risk of epidural hematoma and dural puncture. Patient-specific factors and procedure location significantly influence the incidence and severity of complications for nerve blocks versus epidural anesthesia.
Recovery and Outcomes
Nerve blocks offer targeted pain relief with typically faster initial recovery and fewer side effects compared to epidurals, which involve broader anesthesia and may delay mobilization. Studies show nerve blocks reduce postoperative opioid use and enable earlier rehabilitation, enhancing functional outcomes. Epidurals provide comprehensive pain management effective for extensive surgeries but may increase risks of hypotension and motor blockade, impacting recovery duration.
Nerve block Infographic
 libterm.com
libterm.com