Subarachnoid refers to the space between the arachnoid membrane and the pia mater surrounding the brain and spinal cord, filled with cerebrospinal fluid that cushions and protects the central nervous system. Conditions such as subarachnoid hemorrhage require immediate medical attention due to the risk of severe neurological damage or death. Explore this article to understand the causes, symptoms, and treatment options important for your health.
Table of Comparison
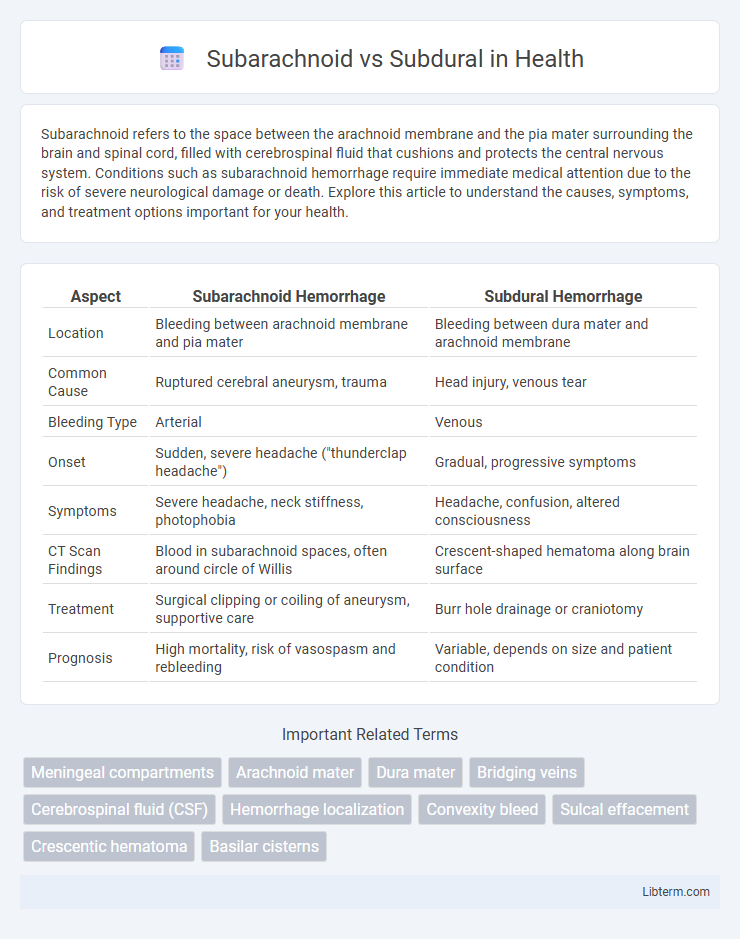
| Aspect | Subarachnoid Hemorrhage | Subdural Hemorrhage |
|---|---|---|
| Location | Bleeding between arachnoid membrane and pia mater | Bleeding between dura mater and arachnoid membrane |
| Common Cause | Ruptured cerebral aneurysm, trauma | Head injury, venous tear |
| Bleeding Type | Arterial | Venous |
| Onset | Sudden, severe headache ("thunderclap headache") | Gradual, progressive symptoms |
| Symptoms | Severe headache, neck stiffness, photophobia | Headache, confusion, altered consciousness |
| CT Scan Findings | Blood in subarachnoid spaces, often around circle of Willis | Crescent-shaped hematoma along brain surface |
| Treatment | Surgical clipping or coiling of aneurysm, supportive care | Burr hole drainage or craniotomy |
| Prognosis | High mortality, risk of vasospasm and rebleeding | Variable, depends on size and patient condition |
Introduction to Intracranial Hemorrhages
Intracranial hemorrhages encompass various types of bleeding within the brain, primarily classified as subarachnoid and subdural hemorrhages. Subarachnoid hemorrhage involves bleeding into the space between the arachnoid membrane and the pia mater, often caused by ruptured cerebral aneurysms, leading to sudden, severe headaches and high morbidity. Subdural hemorrhage occurs between the dura mater and the arachnoid membrane, commonly resulting from traumatic injury that tears bridging veins, with symptoms ranging from acute neurological deficits to chronic complications depending on bleed progression.
Anatomy of Subarachnoid and Subdural Spaces
The subarachnoid space, located between the arachnoid mater and pia mater, contains cerebrospinal fluid (CSF) and major cerebral blood vessels, providing cushioning and nutrient transport for the brain. The subdural space lies between the dura mater and arachnoid mater, often a potential space that can fill with blood or fluid during trauma, causing subdural hematomas. Both spaces are critical in neuroanatomy and pathology, with the subarachnoid space being more involved in CSF circulation and the subdural space more prone to accumulation of pathological fluids.
Causes and Risk Factors
Subarachnoid hemorrhage primarily results from ruptured cerebral aneurysms and arteriovenous malformations, with hypertension and smoking as significant risk factors. Subdural hematomas commonly arise due to traumatic head injuries causing bridging vein tears, especially in elderly patients and those on anticoagulant therapy. Understanding the distinct causes and risk factors of subarachnoid versus subdural hemorrhages aids in accurate diagnosis and targeted prevention strategies.
Pathophysiology: Subarachnoid Hemorrhage
Subarachnoid hemorrhage (SAH) occurs due to bleeding into the subarachnoid space, typically caused by ruptured cerebral aneurysms or arteriovenous malformations, leading to increased intracranial pressure and meningeal irritation. Blood in the cerebrospinal fluid disrupts normal brain function, provoking vasospasm, ischemia, and potential hydrocephalus, contributing to neurological deficits. In contrast, subdural hematomas originate from venous bleeding between the dura mater and arachnoid membrane, usually following trauma, resulting in slower symptom progression compared to the rapid onset seen in SAH.
Pathophysiology: Subdural Hematoma
Subdural hematoma occurs when bridging veins between the brain surface and dura mater rupture, leading to blood accumulation in the subdural space, causing increased intracranial pressure and brain compression. This condition often results from traumatic injury causing venous bleeding, unlike the arterial bleeding seen in subarachnoid hemorrhage. The slow venous bleed in subdural hematoma can cause gradual neurological deterioration, making timely diagnosis and intervention critical.
Clinical Presentation and Symptoms
Subarachnoid hemorrhage typically presents with a sudden, severe headache often described as "thunderclap," accompanied by neck stiffness, photophobia, and possible loss of consciousness due to bleeding in the space between the arachnoid membrane and the pia mater. In contrast, subdural hematoma symptoms develop more gradually, including headache, confusion, drowsiness, and focal neurological deficits from blood accumulation between the dura mater and arachnoid, often following head trauma. Both conditions may cause nausea, vomiting, and altered mental status, but the acute onset in subarachnoid hemorrhage helps differentiate it from the slower progression seen in subdural hematomas.
Diagnostic Imaging and Differentiation
Subarachnoid hemorrhage (SAH) and subdural hematoma (SDH) are differentiated primarily through diagnostic imaging modalities such as CT and MRI. SAH typically appears as hyperdense blood within the subarachnoid space around the brain's sulci and basal cisterns, whereas SDH presents as a crescent-shaped, hyperdense collection along the convexity of the cerebral hemispheres, often crossing suture lines but not dural reflections. CT scans are the first-line imaging choice for acute cases, with MRI providing enhanced detail for subacute or chronic presentations and aiding in distinguishing between these conditions based on location, shape, and density of hemorrhagic collections.
Treatment Approaches and Management
Subarachnoid hemorrhages require immediate management with blood pressure control, surgical clipping or endovascular coiling of aneurysms, and intracranial pressure monitoring to prevent rebleeding and vasospasm. Subdural hematomas often necessitate surgical evacuation through burr hole drainage or craniotomy, especially in acute cases with significant mass effect or neurological decline, alongside supportive care and monitoring for brain swelling. Both conditions demand intensive neurocritical care, but subarachnoid hemorrhages are more closely managed for vascular complications, whereas subdural hematomas focus on relieving mechanical compression.
Prognosis and Complications
Subarachnoid hemorrhage often presents a higher risk of severe complications such as cerebral vasospasm, hydrocephalus, and rebleeding, leading to a prognosis that can be life-threatening with significant neurological deficits. Subdural hematomas generally have a more variable prognosis depending on the acute or chronic nature, with chronic subdural hematomas often showing better outcomes if treated promptly but acute cases carrying risks of increased intracranial pressure and brain herniation. Early diagnosis and intervention are critical in both conditions to minimize long-term neurological damage and improve survival rates.
Prevention and Patient Education
Preventing subarachnoid and subdural hemorrhages involves managing risk factors such as hypertension, anticoagulant use, and head trauma. Patient education should emphasize the importance of wearing helmets during high-risk activities, controlling blood pressure, and recognizing symptoms like sudden severe headache or confusion for early medical intervention. Regular medical check-ups and adherence to prescribed medications reduce the likelihood of bleeding complications in both subarachnoid and subdural spaces.
Subarachnoid Infographic
 libterm.com
libterm.com