Thrombocythemia and leukocytosis are blood disorders characterized by an elevated number of platelets and white blood cells, respectively, often indicating an underlying medical condition or bone marrow issue. Understanding the symptoms, causes, and treatment options for these conditions is crucial for maintaining your overall health and preventing potential complications. Continue reading to explore detailed insights into diagnosis, management, and when to seek medical advice.
Table of Comparison
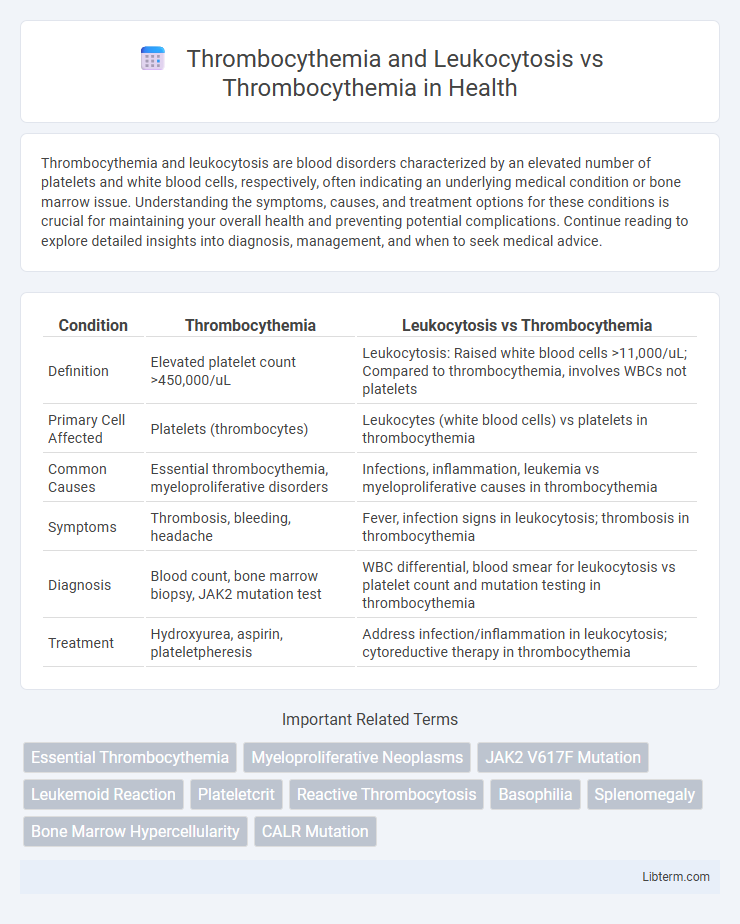
| Condition | Thrombocythemia | Leukocytosis vs Thrombocythemia |
|---|---|---|
| Definition | Elevated platelet count >450,000/uL | Leukocytosis: Raised white blood cells >11,000/uL; Compared to thrombocythemia, involves WBCs not platelets |
| Primary Cell Affected | Platelets (thrombocytes) | Leukocytes (white blood cells) vs platelets in thrombocythemia |
| Common Causes | Essential thrombocythemia, myeloproliferative disorders | Infections, inflammation, leukemia vs myeloproliferative causes in thrombocythemia |
| Symptoms | Thrombosis, bleeding, headache | Fever, infection signs in leukocytosis; thrombosis in thrombocythemia |
| Diagnosis | Blood count, bone marrow biopsy, JAK2 mutation test | WBC differential, blood smear for leukocytosis vs platelet count and mutation testing in thrombocythemia |
| Treatment | Hydroxyurea, aspirin, plateletpheresis | Address infection/inflammation in leukocytosis; cytoreductive therapy in thrombocythemia |
Understanding Thrombocythemia: An Overview
Thrombocythemia involves an abnormal increase in platelet count, often leading to blood clotting disorders, whereas leukocytosis primarily indicates an elevated white blood cell count usually due to infection or inflammation. The distinction lies in the affected blood components: thrombocythemia targets megakaryocyte proliferation in the bone marrow, resulting in excessive platelets, while leukocytosis reflects immune system activation. Understanding thrombocythemia requires recognizing its potential causes, including essential thrombocythemia--a myeloproliferative disorder--and secondary thrombocytosis triggered by conditions such as iron deficiency or chronic inflammation.
What is Leukocytosis? Key Definitions
Leukocytosis is defined as an elevated white blood cell count exceeding the normal range, often indicating an immune response or underlying pathology. It differs from thrombocythemia, which is characterized by an abnormally high platelet count, typically above 450,000 platelets per microliter of blood. While thrombocythemia primarily affects clotting mechanisms, leukocytosis signals enhanced leukocyte activity, frequently associated with infections, inflammation, or hematologic disorders.
Thrombocythemia vs Thrombocythemia with Leukocytosis
Thrombocythemia with leukocytosis presents a distinct hematologic profile characterized by elevated platelet counts alongside increased white blood cell levels, indicating a more complex myeloproliferative disorder often linked to conditions such as primary myelofibrosis or chronic myeloid leukemia. In contrast, isolated thrombocythemia is primarily associated with essential thrombocythemia, where platelet proliferation occurs independently without leukocyte elevation. The presence of leukocytosis in thrombocythemia patients signals a heightened risk for thrombosis and disease progression, necessitating targeted diagnostic and therapeutic strategies.
Causes of Thrombocythemia: Primary and Secondary Factors
Thrombocythemia, characterized by an elevated platelet count, stems from primary causes such as essential thrombocythemia--a myeloproliferative neoplasm driven by genetic mutations like JAK2, CALR, or MPL--and secondary causes including reactive thrombocytosis due to inflammation, infection, iron deficiency, or malignancy. Leukocytosis often co-occurs with secondary thrombocythemia as both respond to inflammatory cytokines and stress stimuli, whereas primary thrombocythemia occurs independently of leukocyte elevation. Differentiating primary from secondary thrombocythemia is crucial for targeted management, relying on bone marrow biopsy, molecular testing, and evaluation of clinical context.
Pathophysiology of Leukocytosis in Thrombocythemia
Leukocytosis in thrombocythemia results from the hyperproliferative activity of hematopoietic stem cells in the bone marrow, driven by mutations such as JAK2 V617F, MPL, or CALR. This mutation-induced dysregulation leads to increased granulocyte proliferation alongside megakaryocyte expansion, causing concurrent elevations in white blood cell and platelet counts. The pathophysiology involves abnormal cytokine signaling pathways, promoting both thrombocytosis and leukocytosis, which distinguishes it from isolated thrombocythemia.
Clinical Manifestations: Differences and Similarities
Thrombocythemia presents with elevated platelet counts leading to symptoms such as thrombosis, erythromelalgia, and bleeding, whereas leukocytosis involves increased white blood cells often linked to infections or inflammation, manifesting as fever and malaise. Both conditions may share manifestations such as splenomegaly and vascular complications, but leukocytosis typically lacks the pronounced thrombotic events seen in thrombocythemia. Clinical evaluation of platelet function and differential blood count is essential to distinguish thrombocythemia from leukocytosis and guide appropriate management.
Diagnostic Criteria for Thrombocythemia and Leukocytosis
Thrombocythemia diagnosis requires a sustained platelet count above 450,000/uL combined with bone marrow examination showing increased megakaryocytes and exclusion of secondary causes. Leukocytosis diagnostic criteria involve a white blood cell count exceeding 11,000/uL, with attention to differential counts to identify neutrophilia, lymphocytosis, or other subtypes. Differentiating Thrombocythemia with Leukocytosis from isolated Thrombocythemia depends on integrated hematologic analysis, including peripheral blood smear, cytogenetics, and molecular markers such as JAK2, CALR, or MPL mutations.
Risk Assessment: Complications and Prognosis
Thrombocythemia combined with leukocytosis significantly increases the risk of thrombotic events, including stroke and myocardial infarction, compared to thrombocythemia alone. Elevated white blood cell counts act as an independent prognostic factor, exacerbating vascular complications and contributing to a higher incidence of disease progression to myelofibrosis or acute leukemia. Risk stratification models incorporate leukocyte levels for more accurate prediction of patient outcomes and guide therapeutic interventions.
Treatment Approaches: Thrombocythemia Alone vs with Leukocytosis
Treatment approaches for thrombocythemia alone primarily involve cytoreductive therapy using hydroxyurea or anagrelide to reduce platelet counts, alongside low-dose aspirin to minimize thrombotic risk. When thrombocythemia coexists with leukocytosis, management intensifies due to higher thrombotic and inflammatory risks, often requiring combination therapy targeting both elevated platelets and white blood cells, with stricter monitoring of hematologic parameters. Emerging treatments may include JAK2 inhibitors like ruxolitinib, particularly in cases with myeloproliferative neoplasm mutations, optimizing control of both cellular proliferations.
Monitoring and Follow-up Strategies
Effective monitoring of thrombocythemia and leukocytosis involves regular complete blood counts (CBC) to track platelet and white blood cell levels, detecting any shifts indicative of disease progression or treatment response. Follow-up strategies for thrombocythemia prioritize periodic assessments of thrombotic risk markers, such as JAK2 V617F mutation status and platelet function tests, to tailor cytoreductive therapy and prevent complications. Leukocytosis management requires vigilant evaluation of underlying causes via differential white cell counts and inflammatory markers, ensuring timely intervention and adjustment of therapeutic regimens based on dynamic hematologic parameters.
Thrombocythemia and Leukocytosis Infographic
 libterm.com
libterm.com