Vasculitis is an inflammatory condition affecting blood vessels, leading to changes such as thickening, weakening, or scarring that can disrupt blood flow and result in organ damage. Early diagnosis and targeted treatment are crucial to manage symptoms and prevent serious complications. Discover more about the types, symptoms, and treatment options to better understand how vasculitis may impact Your health.
Table of Comparison
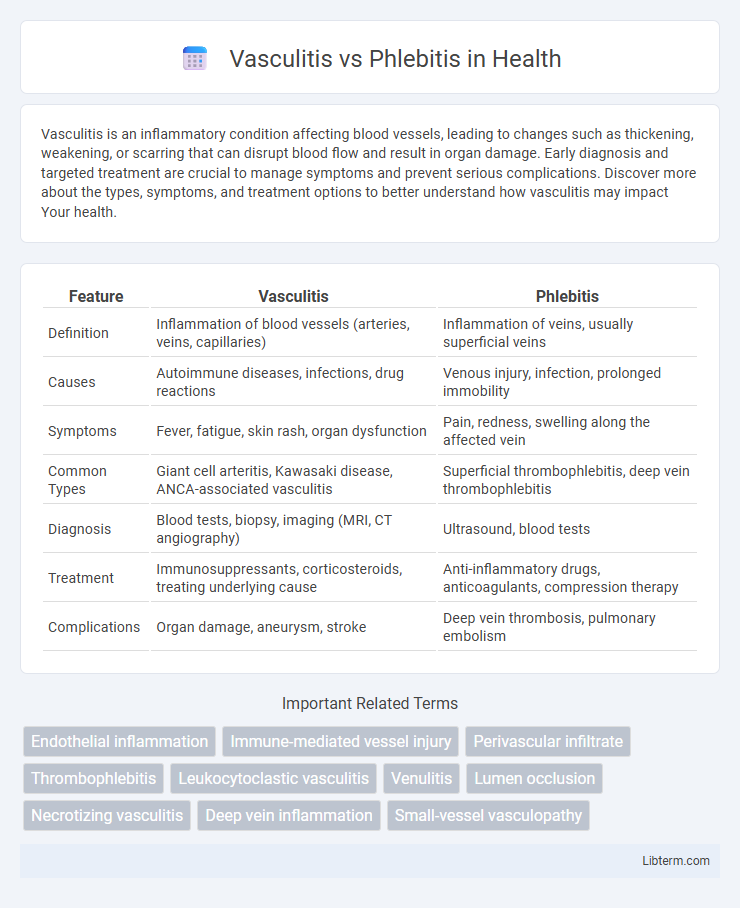
| Feature | Vasculitis | Phlebitis |
|---|---|---|
| Definition | Inflammation of blood vessels (arteries, veins, capillaries) | Inflammation of veins, usually superficial veins |
| Causes | Autoimmune diseases, infections, drug reactions | Venous injury, infection, prolonged immobility |
| Symptoms | Fever, fatigue, skin rash, organ dysfunction | Pain, redness, swelling along the affected vein |
| Common Types | Giant cell arteritis, Kawasaki disease, ANCA-associated vasculitis | Superficial thrombophlebitis, deep vein thrombophlebitis |
| Diagnosis | Blood tests, biopsy, imaging (MRI, CT angiography) | Ultrasound, blood tests |
| Treatment | Immunosuppressants, corticosteroids, treating underlying cause | Anti-inflammatory drugs, anticoagulants, compression therapy |
| Complications | Organ damage, aneurysm, stroke | Deep vein thrombosis, pulmonary embolism |
Understanding Vasculitis: Definition and Overview
Vasculitis is an inflammatory condition affecting the blood vessel walls, leading to changes such as thickening, weakening, narrowing, or scarring. It involves the immune system mistakenly attacking blood vessels, disrupting blood flow and potentially damaging organs. Unlike phlebitis, which specifically refers to inflammation of the veins, vasculitis can impact arteries, veins, and capillaries throughout the body.
What Is Phlebitis? Key Characteristics
Phlebitis is the inflammation of a vein, often caused by infection, injury, or irritation from intravenous catheters. Key characteristics include redness, warmth, swelling, and tenderness along the affected vein, most commonly seen in the legs or arms. Unlike vasculitis, which affects both arteries and veins and involves autoimmune mechanisms, phlebitis primarily targets superficial veins and is frequently associated with blood clot formation, known as thrombophlebitis.
Causes and Risk Factors: Vasculitis vs Phlebitis
Vasculitis is primarily caused by autoimmune disorders, infections, and certain medications, with risk factors including genetic predisposition and chronic inflammatory diseases. Phlebitis results from vein inflammation due to injury, infection, or blood clots, with higher risk related to prolonged immobility, intravenous catheter use, and varicose veins. Both conditions involve inflammation but differ in underlying triggers and affected vessel types, with vasculitis targeting blood vessel walls broadly and phlebitis specifically affecting veins.
Common Symptoms: How to Recognize Each Condition
Vasculitis primarily presents with systemic symptoms such as fever, fatigue, and muscle pain, alongside skin manifestations like purpura and ulcers caused by vessel inflammation. Phlebitis typically features localized pain, redness, swelling, and warmth along the affected vein, often accompanied by a palpable cord. Recognizing vasculitis involves noting widespread inflammation signs and multiorgan impact, whereas phlebitis is identified by superficial vein tenderness and inflammation.
Types of Vasculitis and Phlebitis Explained
Vasculitis encompasses a range of disorders characterized by inflammation of blood vessels, including types such as giant cell arteritis, polyarteritis nodosa, and microscopic polyangiitis, each affecting vessels of varying sizes. Phlebitis specifically refers to inflammation of the veins, most commonly manifesting as superficial thrombophlebitis or deep vein thrombosis, with the latter posing significant risks for embolism. Differentiating these conditions relies on understanding their distinct vascular targets and pathological features, which guides appropriate clinical management and treatment strategies.
Diagnostic Methods: Identifying the Differences
Diagnostic methods for vasculitis primarily include blood tests such as antineutrophil cytoplasmic antibodies (ANCA) and biopsy of affected tissues to detect inflammation in vessel walls. Phlebitis diagnosis often relies on Doppler ultrasound imaging to visualize vein inflammation and assess blood flow abnormalities. Accurate differentiation hinges on histopathological evaluation and specific serological markers to distinguish systemic vasculitis from localized vein inflammation characteristic of phlebitis.
Treatment Approaches: Management Strategies Compared
Treatment approaches for vasculitis focus on suppressing the immune system using corticosteroids and immunosuppressive agents such as cyclophosphamide or methotrexate to reduce blood vessel inflammation and prevent organ damage. In contrast, phlebitis management primarily involves anti-inflammatory measures, including nonsteroidal anti-inflammatory drugs (NSAIDs), warm compresses, and anticoagulants to prevent clot formation in inflamed veins. Both conditions require tailored therapies based on severity and underlying causes, with vasculitis often demanding more aggressive and prolonged immunosuppressive treatment compared to the typically localized and symptomatic care for phlebitis.
Complications and Potential Health Risks
Vasculitis involves inflammation of blood vessel walls, leading to complications such as organ damage, aneurysms, and tissue necrosis due to impaired blood flow. Phlebitis, primarily affecting veins, can result in thrombophlebitis, causing vein clot formation that increases the risk of deep vein thrombosis and pulmonary embolism. Both conditions require prompt diagnosis and treatment to mitigate severe health risks including chronic pain, ischemia, and systemic inflammation.
Prevention and Lifestyle Modifications
Preventing vasculitis and phlebitis involves maintaining a healthy lifestyle that includes regular exercise, balanced nutrition, and avoiding smoking to reduce inflammation and improve vascular health. Managing underlying conditions such as autoimmune disorders and infections through proper medical treatment can significantly lower the risk of vasculitis. For phlebitis, promoting proper blood circulation by staying hydrated, elevating legs when possible, and avoiding prolonged immobility are key preventive strategies.
When to Seek Medical Attention
Seek medical attention immediately for vasculitis if symptoms include unexplained fever, persistent fatigue, weight loss, or signs of organ involvement such as chest pain or neurological deficits. In cases of phlebitis, urgent care is necessary when there is significant leg swelling, redness, warmth along the vein, or intense pain indicating possible deep vein thrombosis. Early diagnosis and treatment are crucial to prevent complications like tissue damage in vasculitis and clot propagation in phlebitis.
Vasculitis Infographic
 libterm.com
libterm.com