Hypomagnesemia, characterized by low magnesium levels in the blood, can lead to symptoms like muscle cramps, fatigue, and abnormal heart rhythms. This condition often results from inadequate dietary intake, gastrointestinal disorders, or certain medications interfering with magnesium absorption. Discover more about the causes, symptoms, diagnosis, and treatment options to protect your health in the rest of this article.
Table of Comparison
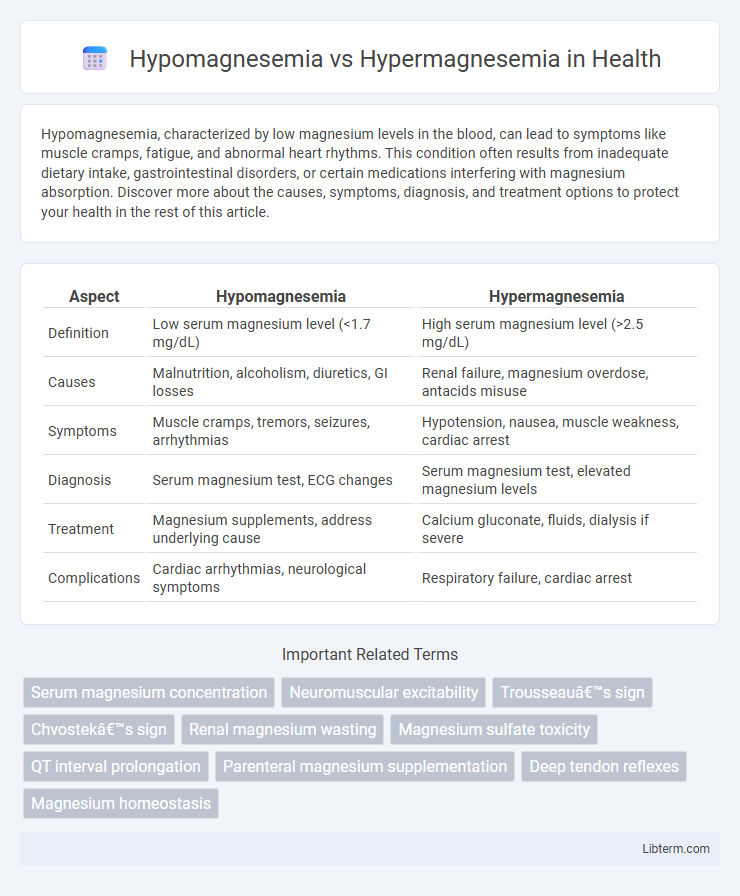
| Aspect | Hypomagnesemia | Hypermagnesemia |
|---|---|---|
| Definition | Low serum magnesium level (<1.7 mg/dL) | High serum magnesium level (>2.5 mg/dL) |
| Causes | Malnutrition, alcoholism, diuretics, GI losses | Renal failure, magnesium overdose, antacids misuse |
| Symptoms | Muscle cramps, tremors, seizures, arrhythmias | Hypotension, nausea, muscle weakness, cardiac arrest |
| Diagnosis | Serum magnesium test, ECG changes | Serum magnesium test, elevated magnesium levels |
| Treatment | Magnesium supplements, address underlying cause | Calcium gluconate, fluids, dialysis if severe |
| Complications | Cardiac arrhythmias, neurological symptoms | Respiratory failure, cardiac arrest |
Introduction to Magnesium Homeostasis
Magnesium homeostasis is critical for maintaining cellular functions, involving precise regulation of magnesium absorption, distribution, and excretion to keep serum magnesium levels within the normal range of 1.7 to 2.2 mg/dL. Hypomagnesemia occurs when serum magnesium drops below 1.7 mg/dL, often resulting from gastrointestinal loss, renal wasting, or inadequate intake, causing neuromuscular and cardiovascular disturbances. Hypermagnesemia, defined by serum magnesium levels above 2.2 mg/dL, typically arises from impaired renal excretion or excessive magnesium intake, leading to muscle weakness, hypotension, and cardiac arrhythmias.
Definition: Hypomagnesemia vs Hypermagnesemia
Hypomagnesemia is defined by abnormally low serum magnesium levels, typically below 1.7 mg/dL, which disrupts cellular functions and neuromuscular activities. Hypermagnesemia occurs when serum magnesium concentrations exceed 2.5 mg/dL, often resulting from excessive magnesium intake or impaired renal excretion, leading to symptoms like muscle weakness and cardiac abnormalities. Both conditions reflect critical imbalances in magnesium homeostasis requiring targeted clinical management.
Causes of Hypomagnesemia
Hypomagnesemia, characterized by low serum magnesium levels often below 1.7 mg/dL, primarily results from gastrointestinal losses such as chronic diarrhea, malabsorption syndromes, and prolonged proton pump inhibitor use. Renal causes include diuretic therapy, hyperaldosteronism, and genetic disorders like Gitelman syndrome leading to excessive urinary magnesium excretion. Other significant causes involve alcoholism, malnutrition, and certain endocrine disorders including uncontrolled diabetes mellitus causing osmotic diuresis and magnesium depletion.
Causes of Hypermagnesemia
Hypermagnesemia occurs primarily due to impaired renal function, as kidneys are unable to excrete excess magnesium effectively, leading to accumulation in the blood. Other causes include excessive intake of magnesium-containing medications such as antacids and laxatives, as well as conditions like adrenal insufficiency and hypothyroidism that disrupt magnesium metabolism. Rarely, excessive magnesium administration during medical treatments or magnesium sulfate overdose can also result in hypermagnesemia.
Clinical Manifestations of Hypomagnesemia
Hypomagnesemia typically presents with neuromuscular symptoms such as muscle cramps, tremors, and tetany, alongside cardiovascular manifestations like arrhythmias and hypertension. Patients may also experience seizures, personality changes, and refractory hypokalemia or hypocalcemia due to impaired parathyroid hormone secretion. In contrast, hypermagnesemia often causes hypotension, diminished deep tendon reflexes, and respiratory depression, highlighting the opposing clinical profiles of these magnesium imbalances.
Clinical Manifestations of Hypermagnesemia
Hypermagnesemia often presents with muscle weakness, hypotension, and respiratory depression due to impaired neuromuscular transmission. Cardiac effects include bradycardia, prolonged PR interval, and potential cardiac arrest in severe cases. Neurological symptoms such as lethargy, confusion, and diminished deep tendon reflexes commonly occur in elevated serum magnesium levels above 4 mg/dL.
Diagnostic Evaluation and Laboratory Findings
Hypomagnesemia is diagnosed through serum magnesium levels below 1.7 mg/dL, often accompanied by low serum calcium and potassium, while hypermagnesemia shows levels above 2.5 mg/dL, frequently linked to renal failure or excessive magnesium intake. Electrolyte panels, renal function tests, and assessment of clinical symptoms such as muscle weakness or cardiac arrhythmias are essential in differential diagnosis. Urinary magnesium excretion and serum magnesium concentrations guide evaluation by distinguishing between renal and non-renal causes of magnesium imbalance.
Treatment Strategies for Hypomagnesemia
Treatment strategies for hypomagnesemia primarily involve magnesium replacement through oral supplements such as magnesium oxide or magnesium gluconate for mild cases, while severe hypomagnesemia requires intravenous magnesium sulfate administration. Monitoring serum magnesium levels and renal function is crucial during therapy to prevent magnesium toxicity and ensure effective restoration. Addressing underlying causes like gastrointestinal losses or medication side effects enhances treatment success and prevents recurrence.
Treatment Strategies for Hypermagnesemia
Treatment strategies for hypermagnesemia primarily involve intravenous administration of calcium gluconate to antagonize the effects of magnesium on cardiac and neuromuscular receptors. Enhancing renal magnesium excretion through diuretics such as loop diuretics, combined with intravenous fluids, helps reduce serum magnesium levels efficiently. In severe cases or when renal function is impaired, hemodialysis is the preferred intervention to rapidly remove excess magnesium from the bloodstream.
Prevention and Prognosis
Preventing hypomagnesemia involves ensuring adequate dietary magnesium intake through foods like nuts, green leafy vegetables, and whole grains, along with monitoring at-risk populations such as those with gastrointestinal disorders or chronic alcoholism. Hypermagnesemia prevention requires cautious use of magnesium-containing medications, especially in patients with renal impairment, and regular serum magnesium monitoring in high-risk groups. Prognosis for hypomagnesemia improves with timely magnesium repletion, while hypermagnesemia prognosis depends on the severity and underlying renal function, with severe cases potentially leading to cardiac complications if untreated.
Hypomagnesemia Infographic
 libterm.com
libterm.com