Cholecystitis and appendicitis are common inflammatory conditions affecting the gallbladder and appendix, respectively, often causing severe abdominal pain and requiring prompt medical attention. Accurate diagnosis through imaging and laboratory tests is crucial for effective treatment, which may include medication or surgery. Explore the rest of the article to understand the symptoms, causes, and best management practices for these conditions to protect your health.
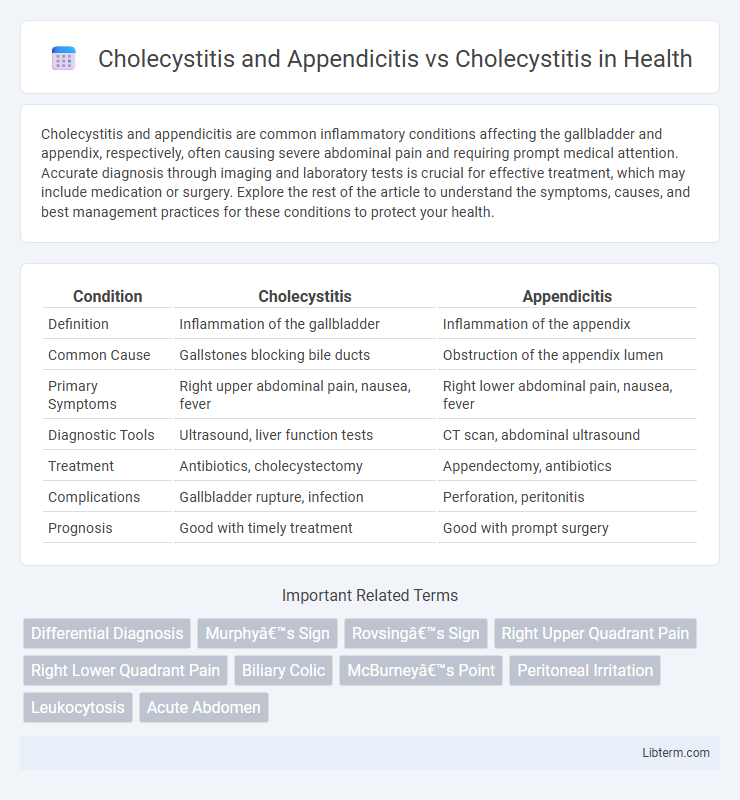
Table of Comparison
| Condition | Cholecystitis | Appendicitis |
|---|---|---|
| Definition | Inflammation of the gallbladder | Inflammation of the appendix |
| Common Cause | Gallstones blocking bile ducts | Obstruction of the appendix lumen |
| Primary Symptoms | Right upper abdominal pain, nausea, fever | Right lower abdominal pain, nausea, fever |
| Diagnostic Tools | Ultrasound, liver function tests | CT scan, abdominal ultrasound |
| Treatment | Antibiotics, cholecystectomy | Appendectomy, antibiotics |
| Complications | Gallbladder rupture, infection | Perforation, peritonitis |
| Prognosis | Good with timely treatment | Good with prompt surgery |
Introduction to Cholecystitis and Appendicitis
Cholecystitis is the inflammation of the gallbladder, typically caused by gallstones blocking the cystic duct, leading to intense abdominal pain and digestive disturbances. Appendicitis involves inflammation of the appendix, often requiring urgent surgical removal to prevent rupture and life-threatening infection. Differentiating these conditions is crucial, as both present with acute abdominal pain but have distinct clinical features, diagnostic criteria, and treatment protocols.
Overview of Cholecystitis
Cholecystitis is the inflammation of the gallbladder, commonly caused by gallstones obstructing the cystic duct, leading to severe abdominal pain, fever, and nausea. It differs from appendicitis, which involves inflammation of the appendix and typically presents with pain localized to the lower right abdomen. Diagnosis of cholecystitis relies on abdominal ultrasound and blood tests showing elevated white blood cells and liver enzymes, while treatment often involves antibiotics and laparoscopic cholecystectomy.
Overview of Appendicitis
Appendicitis is the inflammation of the appendix, often caused by obstruction and infection, leading to severe abdominal pain, typically starting near the navel and shifting to the lower right abdomen. It requires prompt diagnosis and treatment, usually through surgical removal of the appendix (appendectomy), to prevent complications such as rupture and peritonitis. Unlike cholecystitis, which affects the gallbladder and manifests with right upper quadrant pain, appendicitis presents distinct clinical features and diagnostic challenges crucial for effective management.
Cholecystitis and Appendicitis: Key Differences
Cholecystitis involves inflammation of the gallbladder, often caused by gallstones obstructing the cystic duct, leading to intense abdominal pain, fever, and digestive issues. Appendicitis, on the other hand, is inflammation of the appendix, typically resulting from blockage by fecaliths or lymphoid hyperplasia, presenting with sharp pain in the lower right abdomen, nausea, and possible elevated white blood cell count. Both conditions require prompt diagnosis using imaging techniques like ultrasound or CT scan, but treatment differs: cholecystitis often necessitates cholecystectomy, whereas appendicitis requires an appendectomy.
Shared Symptoms and Diagnostic Challenges
Cholecystitis and appendicitis both present with abdominal pain, fever, and elevated white blood cell counts, creating diagnostic challenges due to symptom overlap. Right upper quadrant pain typically suggests cholecystitis, while appendicitis pain often begins periumbilically before localizing to the right lower quadrant, yet atypical presentations can complicate differentiation. Imaging modalities such as ultrasound for cholecystitis and CT scans for appendicitis are critical in distinguishing these conditions to guide appropriate treatment.
Risk Factors Unique to Each Condition
Cholecystitis risk factors uniquely include gallstones, bile duct obstruction, and chronic liver disease, while appendicitis is primarily associated with obstruction of the appendix lumen due to lymphoid hyperplasia or fecaliths. Obesity, female gender, and rapid weight loss are significant for cholecystitis, whereas appendicitis risk is influenced by age, typically affecting younger individuals, and dietary fiber intake. Understanding these distinctions aids in targeted diagnosis and treatment strategies for each condition.
Diagnostic Approaches: Cholecystitis vs. Appendicitis
Cholecystitis diagnosis primarily involves abdominal ultrasound, which detects gallbladder wall thickening, stones, and pericholecystic fluid, while appendicitis diagnosis relies on a combination of clinical scoring systems like the Alvarado score and imaging studies such as ultrasound or CT scan to identify appendiceal inflammation. Laboratory tests for both conditions include elevated white blood cell count and inflammatory markers, but liver function tests may be more indicative in cholecystitis. Timely and specific diagnostic imaging is crucial to distinguish between cholecystitis and appendicitis due to overlapping abdominal pain symptoms, ensuring appropriate treatment selection.
Treatment Modalities for Both Conditions
Treatment modalities for cholecystitis primarily involve antibiotic therapy and laparoscopic cholecystectomy, the surgical removal of the gallbladder, particularly in cases of acute or chronic inflammation. Appendicitis treatment typically includes an appendectomy, either laparoscopic or open, combined with pre- and post-operative antibiotics to manage infection and reduce complications. While both conditions require surgical intervention, cholecystitis management may also involve percutaneous cholecystostomy in high-risk patients, highlighting distinct approaches based on patient status and severity.
Complications and Prognosis Comparison
Cholecystitis can lead to complications such as gallbladder perforation, empyema, and sepsis, while appendicitis risks include rupture, peritonitis, and abscess formation. The prognosis for uncomplicated cholecystitis is generally favorable with timely cholecystectomy, but delayed treatment increases morbidity. Appendicitis requires prompt appendectomy to prevent life-threatening complications, and early intervention usually results in full recovery with low recurrence risk.
Preventive Measures and Patient Education
Cholecystitis and appendicitis both require prompt diagnosis to prevent complications, with preventive measures including maintaining a healthy diet low in saturated fats to reduce gallstone formation and practicing good hygiene to lower the risk of infections causing appendicitis. Patient education emphasizes recognizing early symptoms such as right upper abdominal pain for cholecystitis and lower right abdominal pain for appendicitis, encouraging timely medical evaluation. Lifestyle modifications, including regular exercise and weight management, play a crucial role in minimizing gallbladder disease incidence and supporting overall digestive health.
Cholecystitis and Appendicitis Infographic
 libterm.com
libterm.com