Hypercapnia occurs when excess carbon dioxide builds up in the bloodstream, often due to inadequate respiration or lung disease, leading to symptoms like headache, confusion, and shortness of breath. Elevated CO2 levels can affect your body's pH balance and oxygen delivery, posing serious health risks if untreated. Discover more about the causes, symptoms, and treatments of hypercapnia in the rest of this article.
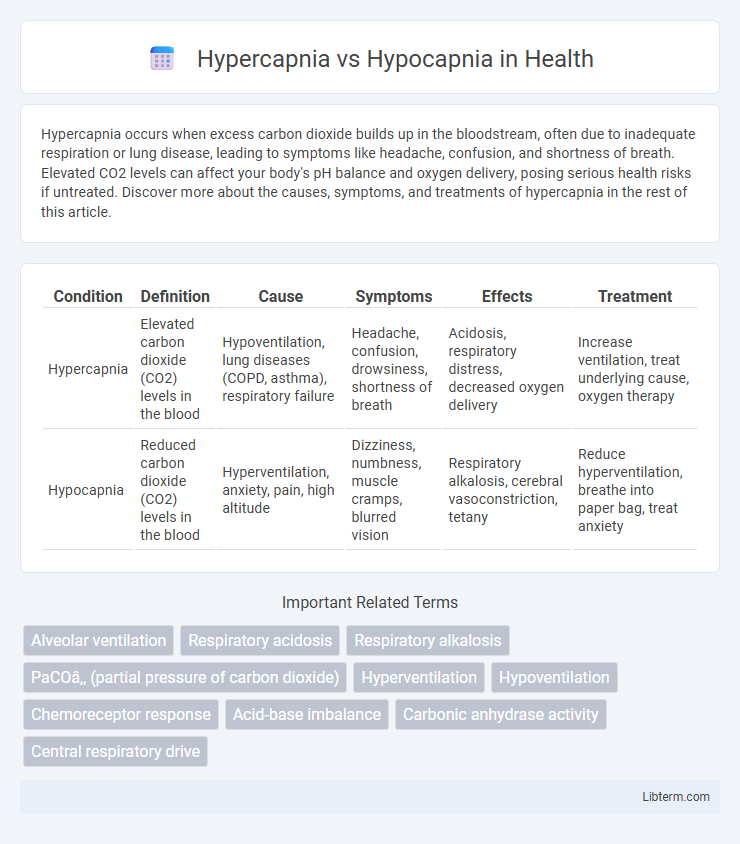
Table of Comparison
| Condition | Definition | Cause | Symptoms | Effects | Treatment |
|---|---|---|---|---|---|
| Hypercapnia | Elevated carbon dioxide (CO2) levels in the blood | Hypoventilation, lung diseases (COPD, asthma), respiratory failure | Headache, confusion, drowsiness, shortness of breath | Acidosis, respiratory distress, decreased oxygen delivery | Increase ventilation, treat underlying cause, oxygen therapy |
| Hypocapnia | Reduced carbon dioxide (CO2) levels in the blood | Hyperventilation, anxiety, pain, high altitude | Dizziness, numbness, muscle cramps, blurred vision | Respiratory alkalosis, cerebral vasoconstriction, tetany | Reduce hyperventilation, breathe into paper bag, treat anxiety |
Introduction to Hypercapnia and Hypocapnia
Hypercapnia refers to an elevated level of carbon dioxide (CO2) in the blood, typically caused by impaired lung function or hypoventilation, while hypocapnia denotes abnormally low CO2 levels, often resulting from hyperventilation. Both conditions disrupt the body's acid-base balance, affecting respiratory and neurological functions. Understanding their distinct physiological impacts is critical for diagnosing disorders like chronic obstructive pulmonary disease (COPD) and anxiety-related hyperventilation.
Definition of Hypercapnia
Hypercapnia is characterized by an elevated level of carbon dioxide (CO2) in the blood, typically exceeding 45 mm Hg, due to inadequate ventilation or impaired gas exchange. This condition contrasts with hypocapnia, which involves abnormally low CO2 levels, often below 35 mm Hg, caused by hyperventilation. Understanding hypercapnia's impact on acid-base balance and respiratory function is crucial for managing respiratory disorders such as chronic obstructive pulmonary disease (COPD) and acute respiratory failure.
Definition of Hypocapnia
Hypocapnia is defined as an abnormally low concentration of carbon dioxide (CO2) in the blood, typically below 35 mmHg, often resulting from hyperventilation. This condition can cause respiratory alkalosis, leading to symptoms such as dizziness, tingling in the extremities, and muscle cramps. In contrast, hypercapnia refers to elevated levels of CO2 in the bloodstream, usually due to inadequate ventilation or lung diseases.
Causes of Hypercapnia
Hypercapnia is caused by inadequate ventilation leading to CO2 retention, commonly seen in chronic obstructive pulmonary disease (COPD), drug overdose affecting respiratory drive, or neuromuscular disorders impairing respiratory muscles. Hypocapnia results from hyperventilation, reducing arterial CO2 levels typically due to anxiety, hypoxia, or metabolic disturbances. Understanding the distinct causes of hypercapnia aids in targeted treatment to restore effective gas exchange and prevent respiratory acidosis.
Causes of Hypocapnia
Hypocapnia primarily results from hyperventilation, which causes excessive carbon dioxide (CO2) expulsion from the bloodstream, leading to decreased arterial CO2 levels. Common causes include anxiety-induced panic attacks, high-altitude exposure, fever, and certain respiratory conditions such as pulmonary embolism or pneumonia that increase breathing rate. Other contributing factors include mechanical ventilation settings and metabolic imbalances affecting respiratory drive.
Signs and Symptoms Comparison
Hypercapnia presents with signs such as headache, confusion, flushed skin, and rapid breathing, reflecting elevated carbon dioxide levels in the blood. Hypocapnia, characterized by low carbon dioxide levels, often causes dizziness, numbness, muscle twitching, and light-headedness. Both conditions affect respiratory and neurological functions but manifest distinctly due to differing carbon dioxide concentrations.
Diagnostic Approaches
Hypercapnia diagnosis primarily involves arterial blood gas (ABG) analysis, revealing elevated partial pressure of carbon dioxide (PaCO2) above 45 mmHg, often complemented by capnography for continuous CO2 monitoring. Hypocapnia is identified through ABG tests showing PaCO2 levels below 35 mmHg, with respiratory rate and clinical evaluation aiding in determining underlying causes such as hyperventilation. Both conditions require pulmonary function tests and imaging studies to assess respiratory mechanics and rule out contributing pathologies.
Clinical Implications and Risks
Hypercapnia, characterized by elevated carbon dioxide levels in the blood, can lead to respiratory acidosis, impaired oxygen delivery, and increased intracranial pressure, posing significant risks in patients with chronic obstructive pulmonary disease (COPD) and acute respiratory distress syndrome (ARDS). Hypocapnia, resulting from reduced carbon dioxide levels, often causes respiratory alkalosis, cerebral vasoconstriction, and decreased oxygen delivery to tissues, increasing the risk of dizziness, syncope, and cerebral hypoxia. Both conditions require careful monitoring of arterial blood gases and prompt intervention to prevent severe complications such as respiratory failure or neurological impairment.
Treatment Strategies for Hypercapnia and Hypocapnia
Treatment strategies for hypercapnia prioritize improving alveolar ventilation through noninvasive ventilation methods such as BiPAP or mechanical ventilation in severe cases to reduce elevated CO2 levels. Hypocapnia treatment focuses on addressing underlying causes like hyperventilation by using breathing techniques or rebreathing into a paper bag to restore normal CO2 concentration, ensuring respiratory alkalosis is corrected. Both conditions require continuous monitoring of arterial blood gases to optimize therapy and prevent complications related to abnormal carbon dioxide levels.
Prevention and Management Tips
Effective prevention of hypercapnia involves ensuring adequate ventilation and avoiding respiratory depressants, while hypocapnia prevention focuses on controlling anxiety and avoiding hyperventilation. Management of hypercapnia includes improving oxygenation, using mechanical ventilation if necessary, and treating underlying respiratory conditions. For hypocapnia, techniques such as breathing into a paper bag, relaxation exercises, and addressing the root cause of excessive breathing help restore normal carbon dioxide levels.
Hypercapnia Infographic
 libterm.com
libterm.com