Chronic obstructive pulmonary disease (COPD) is a progressive lung condition that impairs airflow and causes persistent respiratory symptoms such as coughing, wheezing, and shortness of breath. Effective management focuses on medication, lifestyle changes, and avoiding triggers to improve your breathing and quality of life. Discover more about COPD symptoms, treatments, and prevention strategies in the rest of this article.
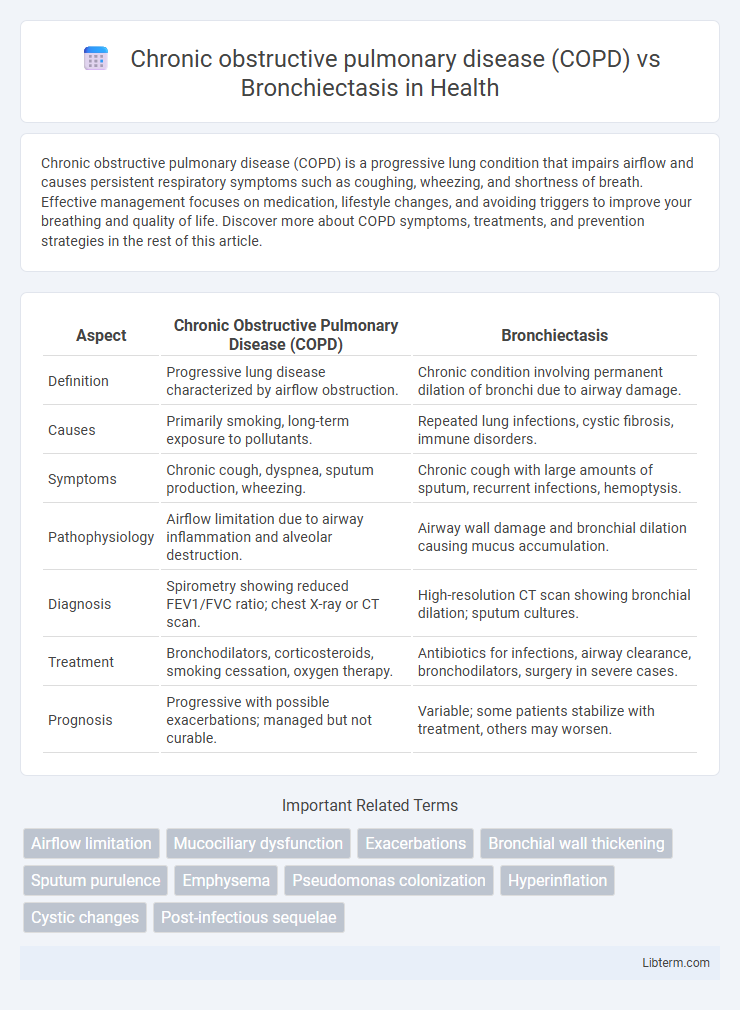
Table of Comparison
| Aspect | Chronic Obstructive Pulmonary Disease (COPD) | Bronchiectasis |
|---|---|---|
| Definition | Progressive lung disease characterized by airflow obstruction. | Chronic condition involving permanent dilation of bronchi due to airway damage. |
| Causes | Primarily smoking, long-term exposure to pollutants. | Repeated lung infections, cystic fibrosis, immune disorders. |
| Symptoms | Chronic cough, dyspnea, sputum production, wheezing. | Chronic cough with large amounts of sputum, recurrent infections, hemoptysis. |
| Pathophysiology | Airflow limitation due to airway inflammation and alveolar destruction. | Airway wall damage and bronchial dilation causing mucus accumulation. |
| Diagnosis | Spirometry showing reduced FEV1/FVC ratio; chest X-ray or CT scan. | High-resolution CT scan showing bronchial dilation; sputum cultures. |
| Treatment | Bronchodilators, corticosteroids, smoking cessation, oxygen therapy. | Antibiotics for infections, airway clearance, bronchodilators, surgery in severe cases. |
| Prognosis | Progressive with possible exacerbations; managed but not curable. | Variable; some patients stabilize with treatment, others may worsen. |
Introduction to COPD and Bronchiectasis
Chronic obstructive pulmonary disease (COPD) is a progressive lung disorder characterized by airflow limitation primarily caused by long-term exposure to noxious particles such as cigarette smoke, leading to chronic bronchitis and emphysema. Bronchiectasis involves permanent dilation of bronchi resulting from chronic infection or inflammation, causing mucus accumulation and recurrent respiratory infections. Both conditions share symptoms like chronic cough and sputum production but differ in pathophysiology, etiology, and treatment approaches.
Epidemiology and Prevalence
Chronic obstructive pulmonary disease (COPD) affects over 300 million people worldwide, ranking as the third leading cause of death globally, with prevalence increasing in smokers and individuals exposed to air pollution. Bronchiectasis, although less common, has seen rising prevalence rates, particularly in older adults and those with a history of respiratory infections or autoimmune diseases. Epidemiological data reveal COPD's widespread impact across high and low-income countries, while bronchiectasis prevalence is often underdiagnosed and varies significantly based on underlying causes and geographic region.
Etiology and Risk Factors
Chronic obstructive pulmonary disease (COPD) primarily results from long-term exposure to cigarette smoke, environmental pollutants, and occupational dust, leading to chronic inflammation and airflow limitation. Bronchiectasis often arises due to recurrent respiratory infections, immune system deficiencies, or genetic conditions like cystic fibrosis, causing permanent bronchial dilation and mucus accumulation. Both diseases share risk factors such as smoking and infections but differ fundamentally in their underlying etiologies and pathophysiological mechanisms.
Pathophysiology Comparison
Chronic obstructive pulmonary disease (COPD) primarily involves progressive airflow limitation caused by chronic inflammation leading to small airway obstruction and alveolar destruction, resulting in emphysema and chronic bronchitis. Bronchiectasis is characterized by permanent dilation and structural damage of the bronchi due to recurrent infections and impaired mucociliary clearance, causing chronic inflammation and mucus accumulation. While COPD's pathophysiology centers on airway remodeling and emphysematous changes, bronchiectasis focuses on bronchial wall damage and abnormal airway dilation.
Clinical Symptoms and Presentation
Chronic obstructive pulmonary disease (COPD) primarily presents with persistent dyspnea, chronic cough, and sputum production, often accompanied by wheezing and episodic exacerbations linked to airflow limitation. Bronchiectasis typically manifests with chronic productive cough, copious purulent sputum, frequent respiratory infections, hemoptysis, and clubbing, reflecting irreversible bronchial dilation and mucus retention. While both conditions share chronic cough and sputum, the severity of sputum production and recurrent infections is markedly higher in bronchiectasis, aiding in clinical differentiation.
Diagnostic Criteria and Tools
Chronic obstructive pulmonary disease (COPD) diagnosis relies on spirometry demonstrating a post-bronchodilator FEV1/FVC ratio below 0.70, along with clinical history of smoking or exposure to noxious particles. Bronchiectasis diagnosis requires high-resolution computed tomography (HRCT) showing irreversible bronchial dilation and clinical features such as chronic productive cough and recurrent respiratory infections. Sputum culture and exacerbation history further support bronchiectasis diagnosis, whereas COPD severity is classified using GOLD criteria based on airflow limitation and symptom assessment.
Imaging Findings: COPD vs Bronchiectasis
Chronic obstructive pulmonary disease (COPD) imaging typically reveals hyperinflation, flattened diaphragms, and increased radiolucency on chest X-rays, with CT scans showing airway wall thickening and emphysematous changes such as centrilobular or paraseptal emphysema. Bronchiectasis imaging is characterized by bronchial dilation exceeding accompanying pulmonary artery diameter, bronchial wall thickening, and lack of bronchial tapering on high-resolution CT, frequently presenting with cystic, varicose, or cylindrical bronchial morphologies. Distinguishing features include air trapping and bullae in COPD versus the pronounced airway wall abnormalities and mucus plugging commonly seen in bronchiectasis on HRCT scans.
Treatment and Management Strategies
Treatment and management strategies for Chronic Obstructive Pulmonary Disease (COPD) primarily include long-acting bronchodilators, inhaled corticosteroids, pulmonary rehabilitation, and oxygen therapy for advanced cases. Bronchiectasis management focuses on airway clearance techniques, antibiotics for bacterial infections, and anti-inflammatory treatments to reduce mucus buildup and prevent exacerbations. Both conditions benefit from smoking cessation, vaccination against respiratory pathogens, and personalized pulmonary care plans to improve lung function and quality of life.
Prognosis and Complications
Chronic obstructive pulmonary disease (COPD) often leads to progressive airflow limitation and increased risk of respiratory infections, with complications including pulmonary hypertension and heart failure, resulting in a variable prognosis depending on disease severity and smoking status. Bronchiectasis is characterized by permanent bronchial dilation and recurrent infections, frequently causing hemoptysis, respiratory failure, and colonization with Pseudomonas aeruginosa, which worsens prognosis. Both conditions significantly impair lung function, but bronchiectasis patients typically experience more frequent exacerbations and require targeted antibiotic therapy to manage chronic infections.
Prevention and Patient Education
Effective prevention of Chronic Obstructive Pulmonary Disease (COPD) centers on smoking cessation, reducing exposure to airborne pollutants, and timely vaccination against respiratory infections like influenza and pneumococcus. Bronchiectasis prevention emphasizes early diagnosis and treatment of respiratory infections, awareness of underlying causes such as cystic fibrosis or immune deficiencies, and regular airway clearance techniques to minimize lung damage. Patient education for both conditions includes promoting adherence to medication regimens, recognizing early symptoms of exacerbations, and maintaining pulmonary rehabilitation efforts to enhance quality of life and reduce hospitalizations.
Chronic obstructive pulmonary disease (COPD) Infographic
 libterm.com
libterm.com