Sialadenitis and mumps both cause inflammation of the salivary glands, leading to painful swelling and difficulty swallowing. While sialadenitis is usually caused by bacterial infection or duct obstruction, mumps is a viral illness that primarily affects children and can cause fever and facial swelling. Explore the rest of this article to understand the causes, symptoms, treatment options, and prevention strategies for these conditions.
Table of Comparison
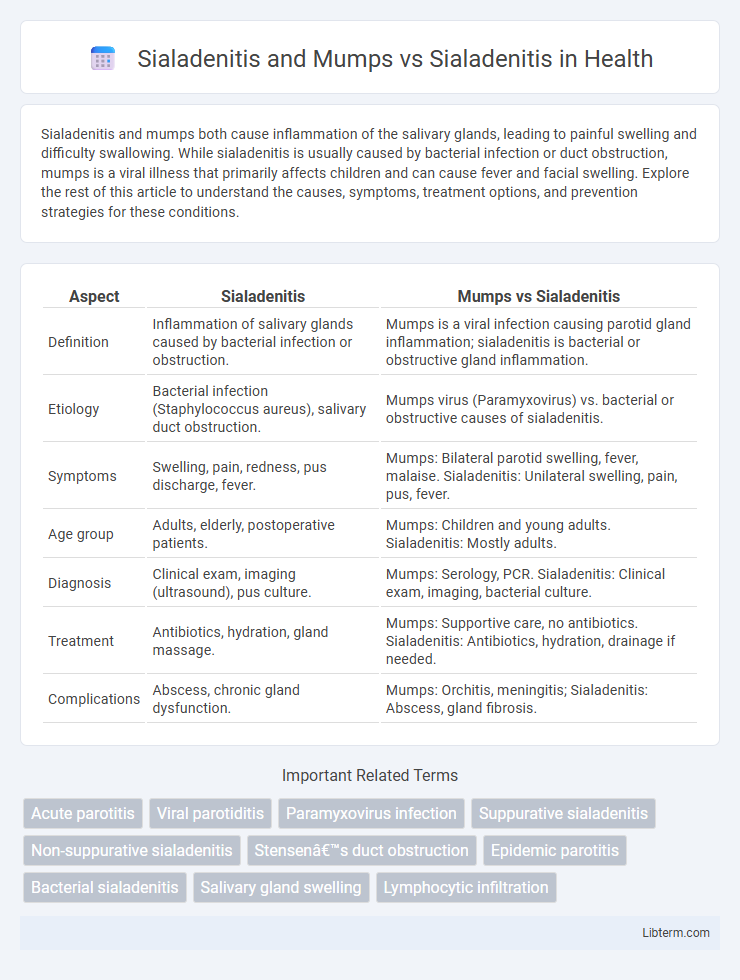
| Aspect | Sialadenitis | Mumps vs Sialadenitis |
|---|---|---|
| Definition | Inflammation of salivary glands caused by bacterial infection or obstruction. | Mumps is a viral infection causing parotid gland inflammation; sialadenitis is bacterial or obstructive gland inflammation. |
| Etiology | Bacterial infection (Staphylococcus aureus), salivary duct obstruction. | Mumps virus (Paramyxovirus) vs. bacterial or obstructive causes of sialadenitis. |
| Symptoms | Swelling, pain, redness, pus discharge, fever. | Mumps: Bilateral parotid swelling, fever, malaise. Sialadenitis: Unilateral swelling, pain, pus, fever. |
| Age group | Adults, elderly, postoperative patients. | Mumps: Children and young adults. Sialadenitis: Mostly adults. |
| Diagnosis | Clinical exam, imaging (ultrasound), pus culture. | Mumps: Serology, PCR. Sialadenitis: Clinical exam, imaging, bacterial culture. |
| Treatment | Antibiotics, hydration, gland massage. | Mumps: Supportive care, no antibiotics. Sialadenitis: Antibiotics, hydration, drainage if needed. |
| Complications | Abscess, chronic gland dysfunction. | Mumps: Orchitis, meningitis; Sialadenitis: Abscess, gland fibrosis. |
Introduction to Sialadenitis
Sialadenitis is an inflammatory condition affecting the salivary glands, often caused by bacterial or viral infections. Common pathogens include Staphylococcus aureus in bacterial sialadenitis and the mumps virus in viral forms, especially in pediatric populations. Distinguishing between mumps-related sialadenitis and other types is crucial for appropriate treatment and prevention of complications.
Overview of Mumps Infection
Mumps is a contagious viral infection primarily affecting the salivary glands, especially the parotid gland, causing painful swelling and inflammation known as mumps sialadenitis. Unlike bacterial sialadenitis, mumps sialadenitis results from the paramyxovirus and presents with systemic symptoms such as fever, headache, and muscle aches. The disease spreads through respiratory droplets, and vaccination with the MMR vaccine is key to prevention, reducing the incidence of mumps-related sialadenitis.
Pathophysiology of Sialadenitis
Sialadenitis is the inflammation of salivary glands caused by bacterial or viral infections, leading to ductal obstruction, decreased saliva flow, and glandular tissue damage. In mumps-induced sialadenitis, the paramyxovirus targets the parotid glands, causing viral replication, cellular swelling, and immune-mediated gland inflammation. Unlike mumps, non-viral sialadenitis often results from bacterial invasion due to saliva stasis and ductal obstruction, resulting in purulent exudate and acute inflammatory responses in glandular tissues.
Causes and Risk Factors
Sialadenitis primarily results from bacterial infections, often caused by Staphylococcus aureus, and is associated with risk factors like dehydration, salivary gland obstruction, and immunosuppression. Mumps-related sialadenitis is caused by the mumps virus, leading to bilateral parotid gland inflammation, particularly in unvaccinated children and young adults. Risk factors for mumps include lack of MMR vaccination, close contact in crowded settings, and seasonal outbreaks during late winter and spring.
Clinical Presentation: Sialadenitis vs Mumps
Sialadenitis presents with acute painful swelling, erythema, and tenderness of the affected salivary gland, often accompanied by purulent discharge from the duct, typically in older adults or those with salivary stasis. Mumps, caused by the paramyxovirus, manifests as bilateral parotid gland swelling with prodromal fever, malaise, myalgia, and rarely purulent discharge, primarily affecting children and adolescents. Distinguishing features include the viral prodrome and bilateral involvement in mumps versus unilateral pain and purulence in bacterial sialadenitis.
Diagnostic Methods and Tools
Sialadenitis diagnosis involves clinical examination, ultrasound imaging, and fine needle aspiration for bacterial culture, distinguishing it from viral infections like mumps, which are primarily confirmed through serological tests and polymerase chain reaction (PCR) assays for mumps virus RNA. Ultrasound reveals gland enlargement and ductal dilation in sialadenitis, whereas mumps typically shows bilateral parotid gland swelling without suppuration. Laboratory findings in sialadenitis include elevated white blood cell count and possible bacterial growth, contrasting with mumps where lymphocytosis and positive IgM antibodies indicate viral infection.
Key Differences: Mumps vs Non-Mumps Sialadenitis
Sialadenitis refers to inflammation of the salivary glands, commonly caused by bacterial infections or obstruction, whereas mumps is a viral infection specifically caused by the mumps virus leading to parotitis. Key differences include the etiology, with mumps being viral and highly contagious, presenting with systemic symptoms like fever and malaise, while non-mumps sialadenitis often involves bacterial pathogens with localized gland pain and purulent discharge. Diagnostic approaches vary: mumps is confirmed via serology or RT-PCR, while non-mumps sialadenitis relies on clinical examination, imaging, and culture of saliva or pus for bacterial identification.
Treatment Approaches and Management
Sialadenitis treatment primarily involves antibiotics targeting bacterial infections, with hydration, warm compresses, and gland massage enhancing recovery, while mumps-related sialadenitis relies on supportive care such as analgesics, antipyretics, and rest due to its viral etiology. Management of bacterial sialadenitis may require surgical drainage if abscesses form, contrasting with mumps management, which focuses on symptom alleviation and isolation to prevent virus spread. Vaccination with MMR significantly reduces mumps incidence, indirectly preventing viral sialadenitis, whereas bacterial sialadenitis prevention emphasizes oral hygiene and prompt treatment of salivary duct obstructions.
Complications and Prognosis
Sialadenitis, an infection or inflammation of the salivary glands, can lead to complications such as abscess formation, glandular necrosis, and chronic sialadenitis if untreated. Mumps-induced sialadenitis, specifically affecting the parotid glands, poses risks of orchitis, meningitis, and hearing loss, complicating prognosis. While idiopathic or bacterial sialadenitis often resolves with antibiotics and supportive care, mumps sialadenitis prognosis depends on immunization status and potential systemic complications, influencing morbidity outcomes.
Prevention and Public Health Measures
Effective prevention of Sialadenitis involves maintaining good oral hygiene, regular hydration, and prompt treatment of bacterial infections to reduce gland inflammation. Mumps vaccination through the MMR (measles, mumps, rubella) vaccine plays a critical role in preventing mumps-induced Sialadenitis, thereby diminishing the incidence of viral salivary gland infections in the population. Public health measures include widespread immunization programs, public awareness campaigns about hygiene practices, and early isolation of infected individuals to limit mumps transmission and associated sialadenitis complications.
Sialadenitis and Mumps Infographic
 libterm.com
libterm.com