Pneumonia is a serious lung infection that causes inflammation in the air sacs, leading to symptoms like coughing, fever, and difficulty breathing. Timely diagnosis and treatment are crucial to prevent complications and ensure a full recovery. Discover more about pneumonia's causes, symptoms, and prevention in the rest of this article.
Table of Comparison
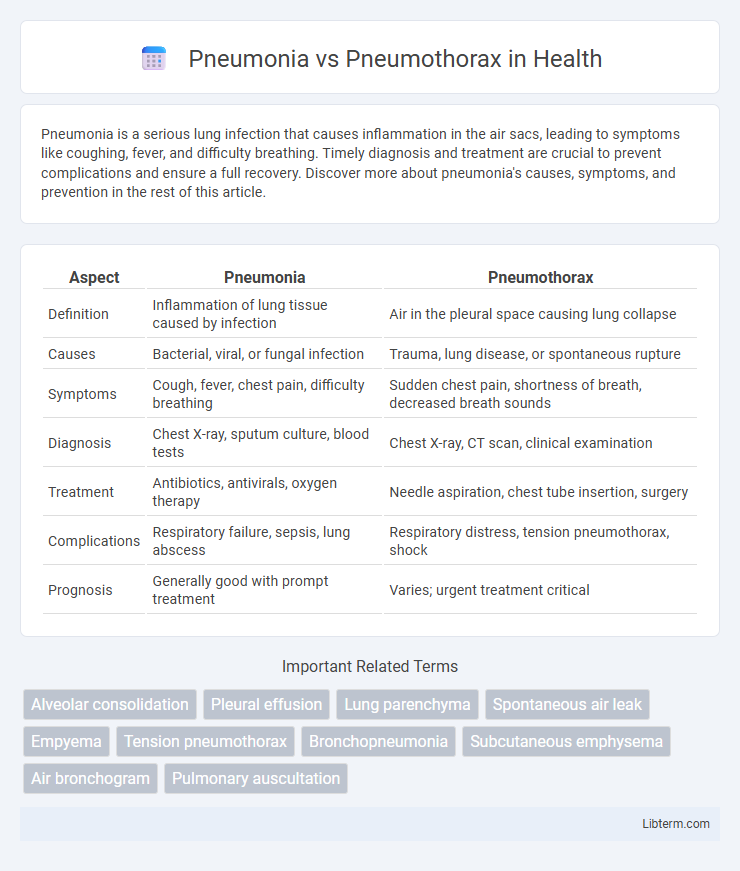
| Aspect | Pneumonia | Pneumothorax |
|---|---|---|
| Definition | Inflammation of lung tissue caused by infection | Air in the pleural space causing lung collapse |
| Causes | Bacterial, viral, or fungal infection | Trauma, lung disease, or spontaneous rupture |
| Symptoms | Cough, fever, chest pain, difficulty breathing | Sudden chest pain, shortness of breath, decreased breath sounds |
| Diagnosis | Chest X-ray, sputum culture, blood tests | Chest X-ray, CT scan, clinical examination |
| Treatment | Antibiotics, antivirals, oxygen therapy | Needle aspiration, chest tube insertion, surgery |
| Complications | Respiratory failure, sepsis, lung abscess | Respiratory distress, tension pneumothorax, shock |
| Prognosis | Generally good with prompt treatment | Varies; urgent treatment critical |
Understanding Pneumonia and Pneumothorax
Pneumonia is an inflammatory lung infection caused by bacteria, viruses, or fungi, characterized by fluid-filled alveoli leading to impaired gas exchange and symptoms such as cough, fever, and chest pain. Pneumothorax involves the presence of air in the pleural cavity, causing lung collapse and resulting in sudden chest pain and shortness of breath. Accurate diagnosis through chest X-rays or CT scans is essential to differentiate between these conditions and provide appropriate treatment to prevent respiratory failure.
Causes and Risk Factors
Pneumonia primarily results from bacterial, viral, or fungal infections that inflame the air sacs in the lungs, commonly caused by Streptococcus pneumoniae, influenza viruses, or aspiration of foreign materials. Pneumothorax occurs when air leaks into the pleural space, often due to chest trauma, underlying lung diseases like chronic obstructive pulmonary disease (COPD), or spontaneous rupture of subpleural blebs in tall, thin individuals. Risk factors for pneumonia include smoking, weakened immune systems, age extremes, and chronic illnesses, whereas pneumothorax risk factors include smoking, prior lung disease, mechanical ventilation, and genetic conditions such as Marfan syndrome.
Key Differences in Pathophysiology
Pneumonia involves inflammation of the lung parenchyma caused by infectious agents such as bacteria, viruses, or fungi, leading to alveolar filling with exudate and impaired gas exchange. Pneumothorax results from the accumulation of air in the pleural space, causing lung collapse due to disrupted negative pressure and impaired lung expansion. Unlike pneumonia, which is primarily an infectious process affecting the lung tissue, pneumothorax is a mechanical issue involving the pleural cavity and lung retraction.
Common Signs and Symptoms
Pneumonia commonly presents with fever, productive cough, chest pain, and dyspnea, accompanied by crackles or decreased breath sounds on auscultation. Pneumothorax is characterized by sudden onset of sharp, unilateral chest pain, shortness of breath, and diminished or absent breath sounds on the affected side, often accompanied by hyperresonance on percussion. Both conditions can cause respiratory distress but differ in etiology and physical exam findings, necessitating prompt differentiation for appropriate management.
Diagnostic Tools and Procedures
Chest X-ray is the primary diagnostic tool for differentiating pneumonia and pneumothorax, revealing lung infiltrates typical of pneumonia or air accumulation in the pleural space indicating pneumothorax. Computed tomography (CT) scans offer detailed imaging to assess lung tissue damage and pleural abnormalities, essential for complex or ambiguous cases. Ultrasonography is increasingly used at the bedside to identify pneumothorax by detecting absence of lung sliding, while sputum cultures and blood tests aid in confirming infectious causes linked to pneumonia.
Treatment Approaches: A Comparative View
Pneumonia treatment primarily involves targeted antibiotic therapy based on the causative pathogen, alongside supportive care such as oxygen supplementation and hydration to manage symptoms. Pneumothorax management varies by severity, with small pneumothoraces often resolving with observation and oxygen therapy, whereas larger or tension pneumothoraces require urgent intervention like needle decompression or chest tube insertion to re-expand the lung. Both conditions necessitate careful monitoring, but the invasive nature of pneumothorax treatment contrasts with the pharmacological and supportive strategies used for pneumonia.
Potential Complications
Pneumonia can lead to complications such as lung abscess, pleural effusion, and acute respiratory distress syndrome (ARDS), which significantly impair gas exchange. Pneumothorax often results in lung collapse causing impaired ventilation, and in tension pneumothorax, it can progress to life-threatening cardiovascular compromise. Both conditions require prompt diagnosis and intervention to prevent severe hypoxemia and respiratory failure.
Prognosis and Recovery
Pneumonia prognosis varies based on factors like age, overall health, and timely antibiotic treatment, with most patients recovering fully within weeks. Pneumothorax recovery depends on the size and cause, with small cases resolving spontaneously and larger ones potentially requiring chest tube insertion; recurrence risk influences long-term outcomes. Both conditions demand prompt medical attention to reduce complications and improve survival rates.
Prevention Strategies
Effective pneumonia prevention strategies include widespread vaccination against Streptococcus pneumoniae and influenza, maintaining good hand hygiene, and avoiding smoking to enhance lung health. Pneumothorax prevention focuses on minimizing risk factors such as avoiding high-risk activities like smoking and managing underlying lung diseases, while immediate medical attention is crucial for spontaneous cases. Both conditions benefit from early detection and lifestyle measures that reduce respiratory complications.
When to Seek Emergency Care
Seek emergency care immediately for pneumonia if experiencing high fever, severe chest pain, difficulty breathing, persistent coughing with blood, or rapid heartbeat, as these may indicate complications or severe infection. For pneumothorax, urgent medical attention is necessary if sudden sharp chest pain and shortness of breath occur, especially if symptoms worsen or are accompanied by cyanosis or confusion, signaling potential lung collapse. Delaying treatment in either condition can lead to life-threatening respiratory failure or sepsis.
Pneumonia Infographic
 libterm.com
libterm.com