Infarction occurs when blood flow to a part of the body is blocked, causing tissue death due to lack of oxygen. Common types include myocardial infarction, often referred to as a heart attack, which requires immediate medical attention to prevent serious complications. Explore the rest of the article to understand symptoms, causes, and treatment options that could be crucial for your health.
Table of Comparison
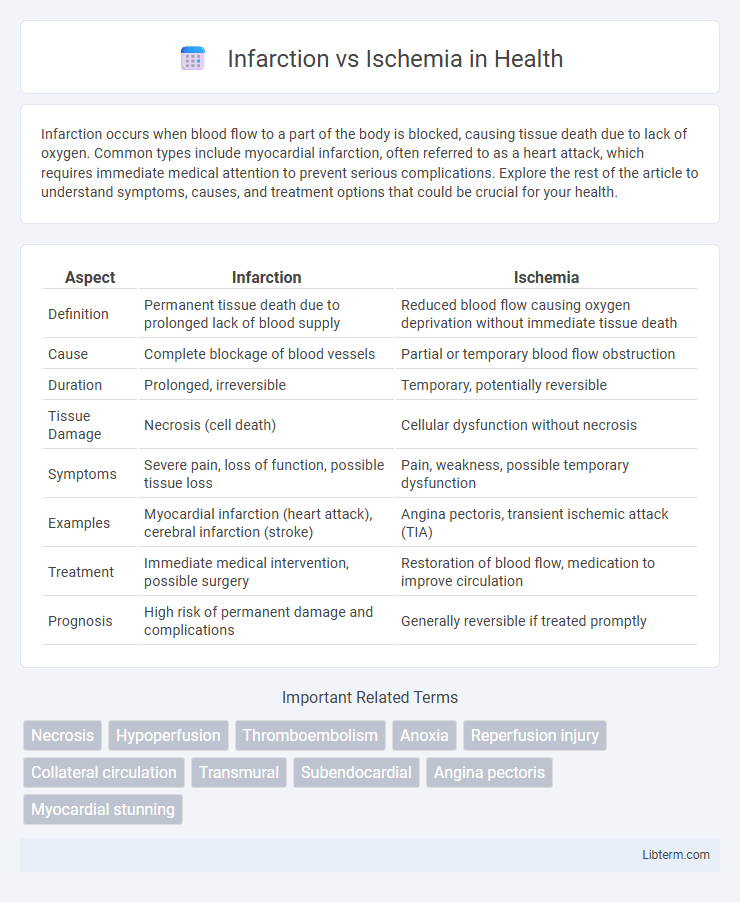
| Aspect | Infarction | Ischemia |
|---|---|---|
| Definition | Permanent tissue death due to prolonged lack of blood supply | Reduced blood flow causing oxygen deprivation without immediate tissue death |
| Cause | Complete blockage of blood vessels | Partial or temporary blood flow obstruction |
| Duration | Prolonged, irreversible | Temporary, potentially reversible |
| Tissue Damage | Necrosis (cell death) | Cellular dysfunction without necrosis |
| Symptoms | Severe pain, loss of function, possible tissue loss | Pain, weakness, possible temporary dysfunction |
| Examples | Myocardial infarction (heart attack), cerebral infarction (stroke) | Angina pectoris, transient ischemic attack (TIA) |
| Treatment | Immediate medical intervention, possible surgery | Restoration of blood flow, medication to improve circulation |
| Prognosis | High risk of permanent damage and complications | Generally reversible if treated promptly |
Introduction to Infarction and Ischemia
Infarction refers to tissue death caused by the prolonged lack of blood supply, often resulting from an obstruction in blood vessels. Ischemia, on the other hand, is the condition of reduced blood flow that deprives tissues of oxygen and nutrients but may not immediately cause cell death. Understanding the distinction between ischemia and infarction is crucial for diagnosing and managing cardiovascular and cerebrovascular diseases.
Defining Infarction: Key Characteristics
Infarction is characterized by the irreversible death of tissue due to prolonged ischemia, where blood supply is critically reduced or completely blocked. This necrosis results from oxygen deprivation and the failure of metabolic processes essential for cell survival. Key markers of infarction include cell swelling, membrane rupture, and inflammatory response, distinguishing it from ischemia, which refers only to reduced blood flow without immediate tissue death.
Understanding Ischemia: An Overview
Ischemia occurs when blood flow to tissues is reduced, leading to insufficient oxygen and nutrient supply, which impairs cellular function. This condition can be temporary or chronic and often affects the heart, brain, and limbs, resulting in pain and tissue dysfunction. Early detection and intervention in ischemia are crucial to prevent progression to infarction, where irreversible tissue death occurs.
Pathophysiological Differences Between Infarction and Ischemia
Infarction is the irreversible death of tissue resulting from prolonged ischemia, where the blood supply is critically reduced or completely obstructed, causing cellular necrosis. Ischemia refers to the reversible reduction in blood flow and oxygen delivery to tissues, leading to metabolic dysfunction without immediate tissue death. Pathophysiologically, ischemia involves a transient imbalance between oxygen supply and demand, whereas infarction marks the point where hypoxia leads to irreversible structural damage and loss of cellular integrity.
Causes and Risk Factors of Infarction
Infarction results from prolonged ischemia causing irreversible tissue death due to complete blockage of blood flow, often triggered by atherosclerosis, thrombosis, or embolism. Key risk factors for infarction include hypertension, smoking, diabetes mellitus, hyperlipidemia, and obesity, which accelerate vascular damage and plaque formation. Understanding these causes and risk factors is crucial for preventing myocardial infarction and stroke.
Causes and Risk Factors of Ischemia
Ischemia occurs when blood flow to tissues is restricted, primarily due to atherosclerosis, thrombosis, or embolism, which reduces oxygen delivery and nutrient supply. Major risk factors contributing to ischemia include hypertension, diabetes mellitus, smoking, hyperlipidemia, and advanced age, all of which promote vascular damage and impaired circulation. Unlike infarction, ischemia may be reversible if blood flow is restored promptly, preventing permanent tissue necrosis.
Clinical Signs and Symptoms: Infarction vs Ischemia
Infarction presents with more severe clinical signs such as intense, persistent pain, localized tissue necrosis, and loss of function, indicating irreversible damage due to complete blood flow obstruction. Ischemia typically manifests as transient pain, pallor, and numbness, reflecting reduced blood supply without immediate tissue death. Early detection of ischemic symptoms is crucial to prevent progression to infarction and permanent organ damage.
Diagnostic Approaches to Infarction and Ischemia
Diagnostic approaches to infarction primarily involve imaging techniques such as cardiac MRI, CT angiography, and echocardiography, which identify tissue necrosis and infarct size. Ischemia diagnosis relies on stress testing, including exercise ECG, nuclear imaging, and myocardial perfusion scans to detect reduced blood flow and reversible tissue hypoxia. Biomarkers like troponins are crucial for infarction detection, while ischemia evaluation emphasizes functional assessment to guide clinical management.
Treatment Strategies: Managing Infarction and Ischemia
Treatment strategies for infarction focus on rapid restoration of blood flow to the affected tissue using thrombolytic therapy, percutaneous coronary intervention (PCI), or surgical revascularization to minimize irreversible damage. Ischemia management involves improving oxygen supply through lifestyle modifications, pharmacologic agents such as nitrates, beta-blockers, and calcium channel blockers, and controlling underlying risk factors like hypertension and diabetes. Early identification and targeted intervention are critical in both conditions to prevent progression from ischemia to infarction and reduce morbidity and mortality rates.
Prognosis and Prevention: Reducing the Risk
Infarction, characterized by irreversible tissue death due to prolonged ischemia, generally carries a poorer prognosis compared to ischemia, where tissue damage is potentially reversible with timely intervention. Effective prevention strategies for both conditions emphasize controlling risk factors such as hypertension, diabetes, smoking cessation, and maintaining a healthy lifestyle to reduce the incidence of arterial blockages. Early detection through regular cardiovascular screenings and the use of antiplatelet or anticoagulant medications significantly lowers the risk of progression from ischemia to infarction.
Infarction Infographic
 libterm.com
libterm.com