Shock is a critical medical condition characterized by insufficient blood flow to the tissues, leading to organ failure and potentially death if untreated. Early recognition and prompt treatment are essential to stabilize circulation and prevent severe complications. Explore the rest of the article to understand the types, symptoms, and life-saving interventions crucial for managing shock.
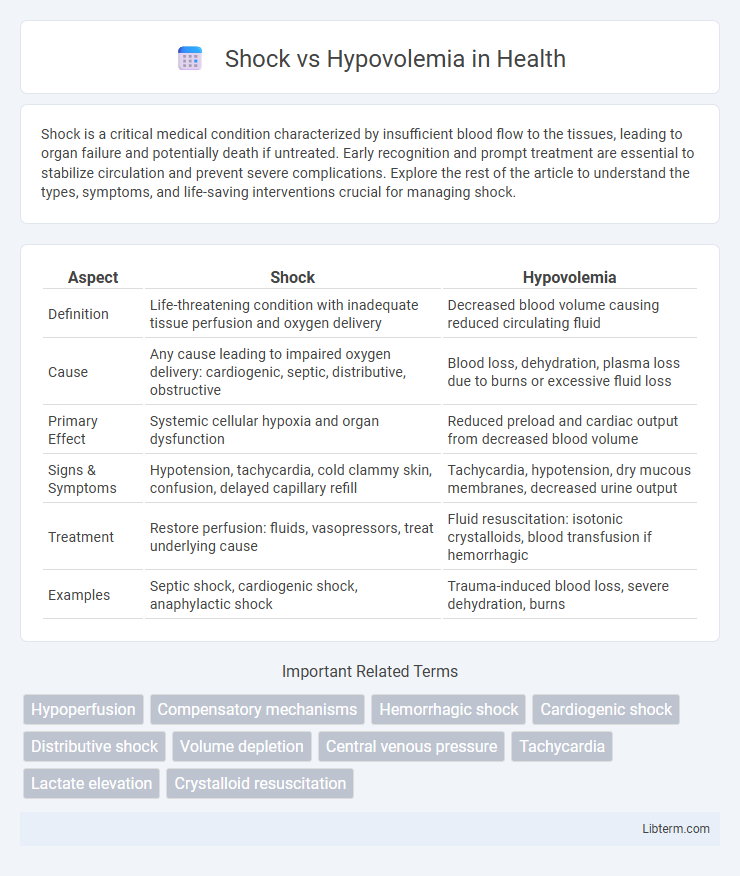
Table of Comparison
| Aspect | Shock | Hypovolemia |
|---|---|---|
| Definition | Life-threatening condition with inadequate tissue perfusion and oxygen delivery | Decreased blood volume causing reduced circulating fluid |
| Cause | Any cause leading to impaired oxygen delivery: cardiogenic, septic, distributive, obstructive | Blood loss, dehydration, plasma loss due to burns or excessive fluid loss |
| Primary Effect | Systemic cellular hypoxia and organ dysfunction | Reduced preload and cardiac output from decreased blood volume |
| Signs & Symptoms | Hypotension, tachycardia, cold clammy skin, confusion, delayed capillary refill | Tachycardia, hypotension, dry mucous membranes, decreased urine output |
| Treatment | Restore perfusion: fluids, vasopressors, treat underlying cause | Fluid resuscitation: isotonic crystalloids, blood transfusion if hemorrhagic |
| Examples | Septic shock, cardiogenic shock, anaphylactic shock | Trauma-induced blood loss, severe dehydration, burns |
Introduction to Shock and Hypovolemia
Shock is a critical condition characterized by inadequate tissue perfusion and oxygen delivery, often resulting from circulatory failure. Hypovolemia, a common cause of shock, involves a significant reduction in blood volume due to hemorrhage, dehydration, or fluid loss, leading to decreased preload and cardiac output. Early recognition and treatment of hypovolemic shock are essential to restore hemodynamic stability and prevent organ dysfunction.
Definitions: Shock vs Hypovolemia
Shock is a life-threatening medical condition characterized by inadequate tissue perfusion and oxygenation, leading to cellular injury and organ dysfunction. Hypovolemia refers to a specific type of shock caused by a significant loss of intravascular fluid volume, resulting in decreased preload, cardiac output, and blood pressure. Differentiating shock from hypovolemia emphasizes the broader pathophysiological mechanisms of shock, which include hypovolemic, cardiogenic, distributive, and obstructive subtypes.
Causes of Shock and Hypovolemia
Shock frequently arises from severe blood loss, trauma, or cardiac dysfunction, impairing tissue perfusion and oxygen delivery. Hypovolemia specifically results from significant fluid or blood volume depletion due to hemorrhage, dehydration, or excessive fluid loss from burns and diarrhea. Both conditions share overlapping causes such as severe bleeding and fluid loss but differ in that shock encompasses broader etiologies including septic, cardiogenic, and neurogenic factors.
Pathophysiology: Key Differences
Shock involves inadequate tissue perfusion and oxygenation due to systemic circulatory failure, leading to cellular dysfunction and metabolic acidosis. Hypovolemia specifically refers to a decreased intravascular volume, causing reduced preload, diminished cardiac output, and subsequent hypotension. The primary pathophysiological difference lies in shock encompassing diverse mechanisms (cardiogenic, distributive, hypovolemic, obstructive), whereas hypovolemia is a distinct cause of shock characterized by volume depletion.
Clinical Presentation and Symptoms
Shock presents with rapid onset of hypotension, tachycardia, cold clammy skin, and altered mental status due to inadequate tissue perfusion. Hypovolemia specifically shows signs of decreased central venous pressure, flattened neck veins, and diminished urine output reflecting intravascular volume loss. Both conditions may exhibit pallor, diaphoresis, and weak pulse, but hypovolemia often includes visible causes like hemorrhage or dehydration.
Diagnostic Criteria and Tools
Shock is diagnosed through a combination of hemodynamic measurements such as blood pressure, heart rate, and tissue perfusion indicators including lactate levels and capillary refill time, while hypovolemia diagnosis centers on clinical signs like decreased skin turgor, dry mucous membranes, and orthostatic hypotension. Diagnostic tools for shock include arterial blood gas analysis, central venous pressure monitoring, and echocardiography to assess cardiac function, whereas hypovolemia is evaluated using fluid responsiveness tests like passive leg raising and ultrasonographic assessment of inferior vena cava diameter. Both conditions often require rapid bedside assessments combined with laboratory data, including hemoglobin concentration and serum electrolytes, to guide timely and appropriate treatment decisions.
Management Strategies for Shock
Management of shock centers on rapid identification and restoration of tissue perfusion through fluid resuscitation, vasopressor support, and oxygen delivery. Hypovolemic shock specifically requires aggressive intravenous fluid administration, preferably crystalloids or blood products, to restore circulating volume and improve preload. Continuous monitoring of hemodynamic parameters and organ function remains essential to guide therapy and prevent progression to multi-organ failure.
Management Strategies for Hypovolemia
Prompt recognition and rapid fluid resuscitation are critical management strategies for hypovolemia, aiming to restore circulating blood volume and tissue perfusion. Isotonic crystalloids like normal saline or lactated Ringer's solution are preferred initial fluids to expand intravascular volume effectively. Monitoring vital signs, urine output, and laboratory parameters guides ongoing therapy and prevents progression to shock conditions.
Complications and Prognosis
Shock and hypovolemia both lead to insufficient tissue perfusion but differ in underlying causes and clinical implications. Complications of shock include multi-organ failure, acute respiratory distress syndrome (ARDS), and irreversible cellular damage, while hypovolemia primarily causes hypoperfusion and may progress to shock if untreated. Prognosis varies; early recognition and fluid resuscitation in hypovolemia often result in recovery, whereas persistent or untreated shock carries a high risk of mortality and long-term organ dysfunction.
Prevention and Patient Education
Preventing shock and hypovolemia involves prompt identification and management of underlying causes such as bleeding, dehydration, or severe infections. Patients should be educated about recognizing early symptoms like rapid heartbeat, dizziness, and cold extremities to seek immediate medical attention. Maintaining adequate hydration, proper wound care, and regular monitoring of chronic conditions can significantly reduce the risk of developing hypovolemia and subsequent shock.
Shock Infographic
 libterm.com
libterm.com