Syncope occurs when there is a temporary loss of consciousness due to a sudden drop in blood flow to the brain, often triggered by factors such as dehydration, stress, or heart problems. Recognizing the underlying causes and symptoms is crucial for effective treatment and prevention of further episodes. Explore this article to understand how syncope affects your health and what measures you can take to manage it.
Table of Comparison
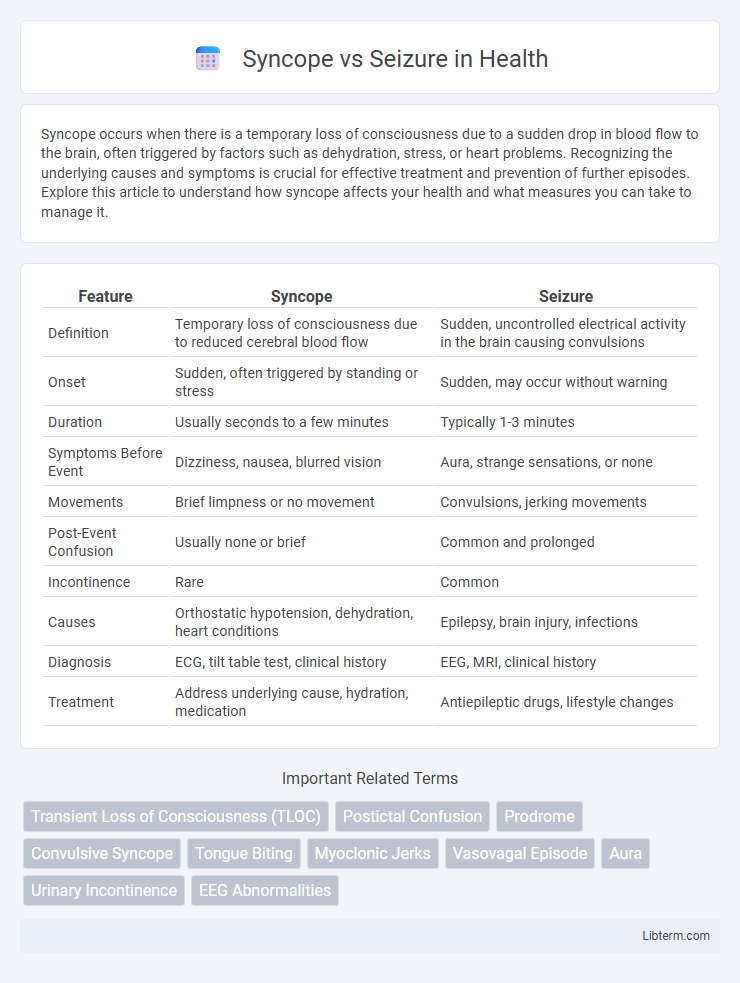
| Feature | Syncope | Seizure |
|---|---|---|
| Definition | Temporary loss of consciousness due to reduced cerebral blood flow | Sudden, uncontrolled electrical activity in the brain causing convulsions |
| Onset | Sudden, often triggered by standing or stress | Sudden, may occur without warning |
| Duration | Usually seconds to a few minutes | Typically 1-3 minutes |
| Symptoms Before Event | Dizziness, nausea, blurred vision | Aura, strange sensations, or none |
| Movements | Brief limpness or no movement | Convulsions, jerking movements |
| Post-Event Confusion | Usually none or brief | Common and prolonged |
| Incontinence | Rare | Common |
| Causes | Orthostatic hypotension, dehydration, heart conditions | Epilepsy, brain injury, infections |
| Diagnosis | ECG, tilt table test, clinical history | EEG, MRI, clinical history |
| Treatment | Address underlying cause, hydration, medication | Antiepileptic drugs, lifestyle changes |
Introduction to Syncope and Seizure
Syncope is a transient loss of consciousness caused by a temporary reduction in cerebral blood flow, often due to cardiovascular or autonomic dysfunction. Seizure, on the other hand, results from abnormal electrical activity in the brain leading to convulsions, sensory disturbances, or altered behavior. Differentiating syncope from seizure is crucial for accurate diagnosis and effective treatment.
Key Differences Between Syncope and Seizure
Syncope is characterized by a temporary loss of consciousness due to reduced cerebral blood flow, often triggered by factors like dehydration or cardiac issues, while seizures result from abnormal electrical activity in the brain. Syncope episodes are typically brief with rapid recovery and lack post-event confusion, whereas seizures often involve prolonged unconsciousness, convulsions, and a postictal state with confusion or fatigue. Diagnosing syncope versus seizure involves evaluating onset, duration, associated symptoms, and diagnostic tests such as EEG for seizures and ECG for syncope to accurately determine the underlying cause.
Causes of Syncope
Syncope is primarily caused by transient cerebral hypoperfusion resulting from factors such as vasovagal responses, orthostatic hypotension, or cardiac arrhythmias, distinguishing it from seizures that originate from abnormal electrical activity in the brain. Common triggers for syncope include dehydration, blood loss, prolonged standing, and autonomic nervous system dysfunction. Understanding these causes is essential for accurate differential diagnosis and effective management between syncope and seizure disorders.
Causes of Seizure
Seizures are caused by abnormal electrical activity in the brain, often triggered by factors such as epilepsy, brain injury, infections like meningitis, or structural brain abnormalities. Metabolic disturbances including hypoglycemia, electrolyte imbalances, and withdrawal from alcohol or drugs can also precipitate seizures. Genetic predisposition and neurodegenerative diseases contribute to seizure occurrence by altering neuronal function and excitability.
Signs and Symptoms: Syncope vs Seizure
Syncope typically presents with sudden transient loss of consciousness, pallor, sweating, and brief muscle weakness, often preceded by lightheadedness or visual disturbances. Seizures manifest as involuntary jerking movements, altered awareness, tongue biting, and postictal confusion, with possible aura symptoms prior to the event. Distinguishing features include rapid recovery in syncope versus prolonged confusion or fatigue following a seizure.
Diagnostic Criteria for Syncope and Seizure
Diagnostic criteria for syncope primarily include a transient loss of consciousness with rapid onset, short duration, and spontaneous complete recovery, often triggered by factors such as standing or emotional stress, alongside signs of global cerebral hypoperfusion. Seizure diagnosis relies on clinical evidence of abnormal, excessive neuronal activity characterized by convulsions, automatisms, or sensory disturbances, supported by electroencephalogram (EEG) findings showing epileptiform discharges. Differentiating features include the presence of postictal confusion in seizures and prodromal symptoms like lightheadedness in syncope, aiding accurate clinical assessment.
Physical Exam Findings
Physical exam findings in syncope often reveal transient hypotension or bradycardia, with normal neurological status and rapid recovery of consciousness. Seizure exams typically show postictal confusion, tongue biting, incontinence, and focal neurological deficits depending on seizure type. Cardiovascular and neurological assessments help differentiate syncope from seizure by identifying arrhythmias or neurologic abnormalities, respectively.
Risk Factors and Triggers
Syncope is commonly triggered by factors such as dehydration, prolonged standing, and sudden postural changes, often influenced by cardiovascular conditions like arrhythmias or orthostatic hypotension. Seizure risk factors include neurological disorders like epilepsy, brain injury, infections, and genetic predispositions, with triggers such as sleep deprivation, flashing lights, and stress. Differentiating these conditions relies on understanding distinct triggers and underlying risk factors, critical for accurate diagnosis and management.
Treatment and Management Options
Treatment for syncope centers on identifying and addressing underlying causes such as dehydration, cardiac issues, or orthostatic hypotension, often involving lifestyle modifications, hydration, and medications like beta-blockers or fludrocortisone. Seizure management typically requires anti-epileptic drugs (AEDs) tailored to seizure type, with options including valproate, lamotrigine, or levetiracetam, alongside lifestyle adjustments and avoiding seizure triggers. Both conditions benefit from thorough diagnostic evaluation to guide personalized therapy and improve patient outcomes.
When to Seek Medical Attention
Seek immediate medical attention if syncope occurs with chest pain, palpitations, severe shortness of breath, or if it results in injury or prolonged unconsciousness. Seizures warrant urgent evaluation when they last longer than five minutes, recur without recovery, or are accompanied by difficulty breathing, confusion, or neurological deficits post-event. Persistent syncope or seizures require prompt specialist assessment to diagnose underlying cardiac, neurological, or metabolic causes and initiate appropriate treatment.
Syncope Infographic
 libterm.com
libterm.com