Sleep disorders disrupt your natural sleep patterns, leading to difficulties in falling asleep, staying asleep, or experiencing restful sleep. Common types include insomnia, sleep apnea, restless legs syndrome, and narcolepsy, each affecting overall health and daily functioning differently. Discover effective treatments and lifestyle changes to improve your sleep quality by reading the rest of this article.
Table of Comparison
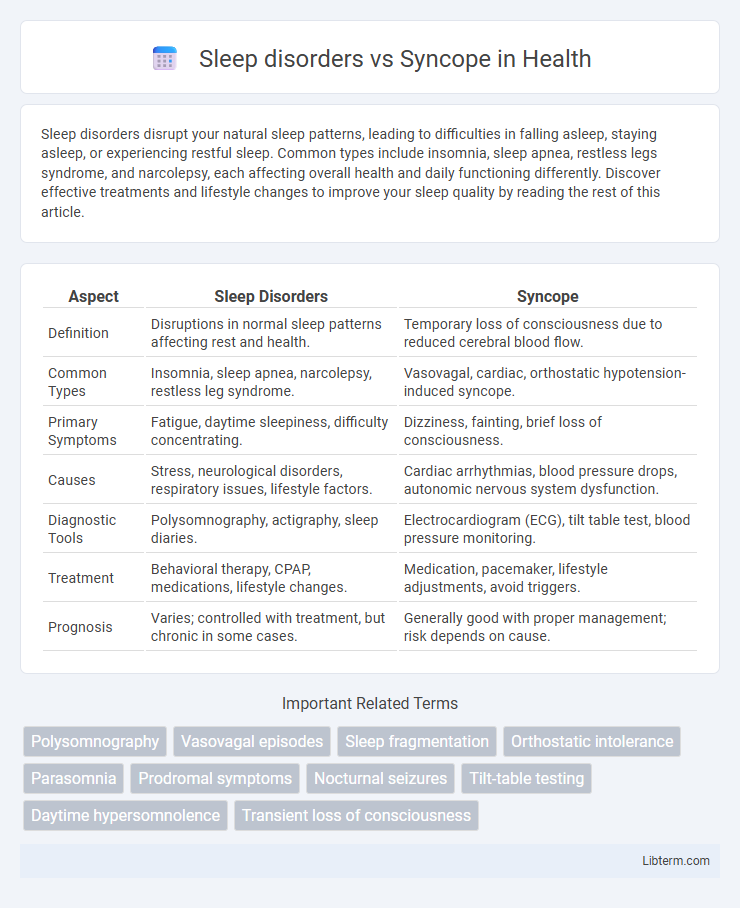
| Aspect | Sleep Disorders | Syncope |
|---|---|---|
| Definition | Disruptions in normal sleep patterns affecting rest and health. | Temporary loss of consciousness due to reduced cerebral blood flow. |
| Common Types | Insomnia, sleep apnea, narcolepsy, restless leg syndrome. | Vasovagal, cardiac, orthostatic hypotension-induced syncope. |
| Primary Symptoms | Fatigue, daytime sleepiness, difficulty concentrating. | Dizziness, fainting, brief loss of consciousness. |
| Causes | Stress, neurological disorders, respiratory issues, lifestyle factors. | Cardiac arrhythmias, blood pressure drops, autonomic nervous system dysfunction. |
| Diagnostic Tools | Polysomnography, actigraphy, sleep diaries. | Electrocardiogram (ECG), tilt table test, blood pressure monitoring. |
| Treatment | Behavioral therapy, CPAP, medications, lifestyle changes. | Medication, pacemaker, lifestyle adjustments, avoid triggers. |
| Prognosis | Varies; controlled with treatment, but chronic in some cases. | Generally good with proper management; risk depends on cause. |
Introduction to Sleep Disorders and Syncope
Sleep disorders encompass a range of conditions characterized by disruptions in normal sleep patterns, including insomnia, sleep apnea, narcolepsy, and restless leg syndrome, which can severely impact cognitive function, mood, and overall health. Syncope, defined as a transient loss of consciousness due to cerebral hypoperfusion, often results from cardiovascular or neurological causes and requires precise differential diagnosis to distinguish from sleep-related phenomena like nocturnal seizures or parasomnias. Understanding the clinical presentation, diagnostic criteria, and pathophysiology of both sleep disorders and syncope is fundamental for effective treatment and improved patient outcomes.
Defining Sleep Disorders
Sleep disorders encompass a range of conditions that disrupt normal sleep patterns, including insomnia, sleep apnea, restless leg syndrome, and narcolepsy. These disorders impair the quality, timing, and duration of sleep, leading to excessive daytime sleepiness, cognitive impairment, and reduced overall health. Unlike syncope, which involves sudden, temporary loss of consciousness due to reduced blood flow to the brain, sleep disorders primarily affect the body's restorative rest cycles and neurological regulation during sleep.
Understanding Syncope: Causes and Mechanisms
Syncope, a temporary loss of consciousness caused by a sudden drop in blood flow to the brain, differs from sleep disorders that primarily affect sleep patterns and quality. Common causes of syncope include vasovagal responses, cardiac arrhythmias, and orthostatic hypotension, with mechanisms involving transient cerebral hypoperfusion. Accurate diagnosis is essential to differentiate syncope from sleep disturbances and to implement appropriate treatments.
Key Differences Between Sleep Disorders and Syncope
Sleep disorders primarily involve disturbances in sleep patterns such as insomnia, sleep apnea, or narcolepsy, characterized by difficulty falling or staying asleep, excessive daytime sleepiness, or abnormal sleep behaviors. Syncope is a transient loss of consciousness caused by a sudden drop in blood flow to the brain, often linked to cardiovascular or neurological conditions and marked by rapid onset and quick recovery. Key differences include that sleep disorders affect the quality and continuity of sleep while syncope results in abrupt blackout episodes unrelated to sleep cycles, requiring distinct diagnostic approaches and treatments.
Common Symptoms: Overlaps and Distinctions
Sleep disorders and syncope share common symptoms such as episodes of sudden loss of consciousness, fatigue, and disorientation, making differential diagnosis challenging. Sleep disorders primarily manifest through disrupted sleep patterns, excessive daytime sleepiness, and snoring, while syncope is characterized by brief, transient fainting spells caused by reduced cerebral blood flow. Accurate assessment of patient history, symptom triggers, and diagnostic tests like polysomnography or tilt-table testing help distinguish between these conditions.
Diagnostic Approaches for Sleep Disorders vs Syncope
Diagnostic approaches for sleep disorders often involve polysomnography, which records brain waves, oxygen levels, and heart rate to identify abnormalities during sleep. Syncope diagnosis relies on patient history, physical examination, ECG monitoring, and sometimes tilt-table testing to assess cardiovascular causes. Differentiating between these conditions requires targeted testing tailored to neurological versus cardiac or hemodynamic factors.
Risk Factors and Demographics
Sleep disorders, including insomnia and sleep apnea, predominantly affect adults aged 40-70, with higher prevalence in males and individuals with obesity, hypertension, or diabetes. Syncope, characterized by sudden transient loss of consciousness, is more common in the elderly population over 70 years, with risk factors such as cardiovascular disease, dehydration, and medication use. Both conditions share overlapping demographics but differ in etiological risk profiles, necessitating tailored diagnostic and management approaches.
Management and Treatment Strategies
Management of sleep disorders involves cognitive-behavioral therapy for insomnia, pharmacological treatments such as sedative-hypnotics, and lifestyle modifications including sleep hygiene improvements. Syncope treatment prioritizes identifying underlying causes through cardiovascular evaluation and may require interventions like pacemaker implantation, medication adjustments, or physical counter-maneuvers to prevent episodes. Both conditions necessitate tailored therapeutic approaches aimed at symptom control and reducing recurrence risk based on individual patient profiles.
Potential Complications and Prognosis
Sleep disorders such as sleep apnea can lead to cardiovascular complications including hypertension, stroke, and heart failure, while syncope, often caused by transient cerebral hypoperfusion, may indicate underlying cardiac or neurological conditions with risks of injury from sudden falls. The prognosis for sleep disorders varies widely, with untreated cases increasing morbidity and mortality rates, whereas syncope prognosis depends on the etiology, where cardiac syncope carries a higher risk of sudden death compared to vasovagal syncope. Both conditions require thorough diagnosis and management to mitigate potential complications and improve patient outcomes.
When to Seek Medical Attention
Persistent or recurrent episodes of unexplained loss of consciousness, especially if accompanied by chest pain, palpitations, or neurological symptoms, warrant immediate medical evaluation to differentiate syncope from sleep disorders. Difficulty maintaining alertness during daily activities or excessive daytime sleepiness that impairs functioning should prompt consultation with a sleep specialist to rule out disorders such as narcolepsy or sleep apnea. Early diagnosis and treatment can prevent serious complications, including injury from falls or cardiovascular events linked to syncope and untreated sleep disorders.
Sleep disorders Infographic
 libterm.com
libterm.com