Platelet aggregation plays a crucial role in coagulation by forming a platelet plug that helps stop bleeding at injury sites. This process involves platelets adhering to damaged blood vessel walls and releasing chemicals that attract more platelets, leading to clot formation. Discover how understanding platelet aggregation can enhance your knowledge of hemostasis and the body's natural defense mechanisms by reading the rest of the article.
Table of Comparison
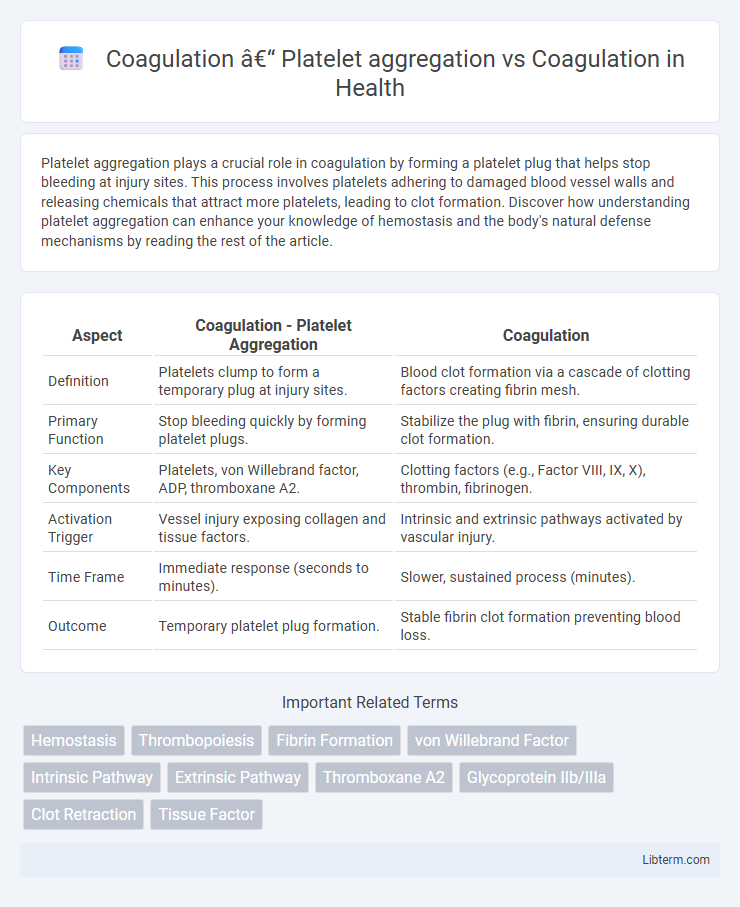
| Aspect | Coagulation - Platelet Aggregation | Coagulation |
|---|---|---|
| Definition | Platelets clump to form a temporary plug at injury sites. | Blood clot formation via a cascade of clotting factors creating fibrin mesh. |
| Primary Function | Stop bleeding quickly by forming platelet plugs. | Stabilize the plug with fibrin, ensuring durable clot formation. |
| Key Components | Platelets, von Willebrand factor, ADP, thromboxane A2. | Clotting factors (e.g., Factor VIII, IX, X), thrombin, fibrinogen. |
| Activation Trigger | Vessel injury exposing collagen and tissue factors. | Intrinsic and extrinsic pathways activated by vascular injury. |
| Time Frame | Immediate response (seconds to minutes). | Slower, sustained process (minutes). |
| Outcome | Temporary platelet plug formation. | Stable fibrin clot formation preventing blood loss. |
Understanding Hemostasis: Coagulation and Platelet Aggregation
Platelet aggregation is the initial phase of hemostasis where platelets adhere to the damaged blood vessel wall and aggregate to form a temporary plug, while coagulation involves a complex cascade of clotting factors that stabilize this plug by converting fibrinogen into fibrin. The interplay between platelet aggregation and the coagulation cascade ensures the formation of a stable blood clot, preventing excessive bleeding. Effective understanding of hemostasis highlights the role of both platelet function and enzymatic pathways in maintaining vascular integrity after injury.
What Is Platelet Aggregation?
Platelet aggregation is the process where platelets clump together to form a blood clot, crucial for stopping bleeding at injury sites. This initial phase of coagulation involves the activation of platelets by signals such as collagen and thrombin, leading to the release of granules that promote further platelet adhesion and aggregation. Unlike the full coagulation cascade that stabilizes the clot with fibrin mesh, platelet aggregation specifically refers to the cellular clumping that forms the primary hemostatic plug.
The Coagulation Cascade Explained
The coagulation cascade is a complex series of enzymatic reactions leading to fibrin clot formation, essential for hemostasis after vascular injury. Platelet aggregation, the clumping of platelets mediated by fibrinogen binding to glycoprotein IIb/IIIa receptors, serves as a critical initial step that stabilizes the developing clot. While platelet aggregation rapidly forms the primary hemostatic plug, the coagulation cascade reinforces it by generating fibrin mesh through intrinsic, extrinsic, and common pathways involving clotting factors such as Factor VIII, IX, X, and thrombin.
Key Differences Between Platelet Aggregation and Coagulation
Platelet aggregation involves the clumping of platelets to form a primary hemostatic plug at the site of vascular injury, whereas coagulation refers to the enzymatic cascade that stabilizes this plug by generating fibrin. Platelet aggregation is primarily mediated by platelet surface receptors like GPIIb/IIIa and soluble agonists such as ADP and thromboxane A2, while coagulation depends on a sequential activation of clotting factors including Factor Xa and thrombin. The key difference lies in platelet aggregation being an immediate cellular response forming a soft clot, whereas coagulation establishes a durable fibrin network that solidifies the clot for long-term vessel repair.
Molecular Mechanisms Involved
Platelet aggregation is initiated by the activation of platelet surface receptors such as GPIIb/IIIa, which bind fibrinogen to form platelet plugs, whereas coagulation involves a complex cascade of enzymatic reactions culminating in the conversion of prothrombin to thrombin and fibrinogen to fibrin to stabilize the clot. Molecular mechanisms of platelet aggregation include signaling pathways triggered by agonists like ADP and thromboxane A2, leading to intracellular calcium mobilization and granule secretion. Coagulation pathways are divided into intrinsic, extrinsic, and common pathways, with key factors such as Factor Xa and Factor Va acting as cofactors in the prothrombinase complex essential for thrombin generation.
Role of Platelets in Blood Clot Formation
Platelets play a critical role in blood clot formation by aggregating at the site of vascular injury to form a primary hemostatic plug, which is essential for stopping bleeding. This platelet aggregation process involves adhesion to the damaged endothelium, activation, and the release of granules that promote further platelet recruitment and stabilization of the clot. Coagulation complements this by generating fibrin strands through a cascade of clotting factors, reinforcing the platelet plug and ensuring durable hemostasis.
Coagulation Factors and Their Functions
Coagulation primarily involves a complex cascade of coagulation factors such as Factor I (fibrinogen), Factor II (prothrombin), and Factor X, which convert fibrinogen into fibrin to stabilize the blood clot. Platelet aggregation initiates clot formation by adhering to damaged endothelium and releasing granules that activate these coagulation factors. Each coagulation factor plays a specific role: Factor VII starts the extrinsic pathway, Factor VIII acts as a cofactor in the intrinsic pathway, and Factor XIII cross-links fibrin strands, ensuring clot stability and wound healing.
Disorders Affecting Platelet Aggregation vs. Coagulation
Disorders affecting platelet aggregation, such as Glanzmann thrombasthenia and Bernard-Soulier syndrome, impair the ability of platelets to clump together, leading to mucocutaneous bleeding and prolonged bleeding time. In contrast, coagulation disorders like hemophilia A and B involve deficiencies in clotting factors VIII or IX, resulting in impaired fibrin clot formation and deep tissue or joint bleeding. Accurate diagnosis differentiates these conditions by evaluating platelet function tests and coagulation factor assays to guide targeted treatment strategies.
Diagnostic Tests: Platelet Function vs. Coagulation Profiling
Diagnostic tests for platelet function primarily include platelet aggregation studies using agents like ADP, collagen, and ristocetin to evaluate platelet responsiveness and aggregation capacity. Coagulation profiling involves assays such as prothrombin time (PT), activated partial thromboplastin time (aPTT), and thrombin time (TT) to assess the integrity of clotting factors and the coagulation cascade. Combining platelet function tests with coagulation profiles provides a comprehensive evaluation of hemostatic disorders, distinguishing between platelet defects and coagulation factor deficiencies.
Therapeutic Implications: Targeting Aggregation or Coagulation
Targeting platelet aggregation primarily involves antiplatelet agents such as aspirin and P2Y12 inhibitors, which prevent thrombus formation in arterial circulation, reducing the risk of myocardial infarction and stroke. Coagulation cascade inhibition, through anticoagulants like direct oral anticoagulants (DOACs) or warfarin, is crucial for managing venous thromboembolism and atrial fibrillation by impairing fibrin clot formation. Selecting between antiplatelet and anticoagulant therapy depends on the pathology's predominance--arterial versus venous thrombosis--with emerging therapies aiming to balance efficacy and bleeding risk by precisely modulating these pathways.
Coagulation – Platelet aggregation Infographic
 libterm.com
libterm.com