Thyroiditis is an inflammation of the thyroid gland that can cause symptoms such as swelling, pain, and changes in hormone levels, leading to either hyperthyroidism or hypothyroidism. Early diagnosis and treatment are crucial for managing symptoms and preventing complications associated with thyroid dysfunction. Discover more about the types, causes, and effective treatments of thyroiditis in the rest of this article.
Table of Comparison
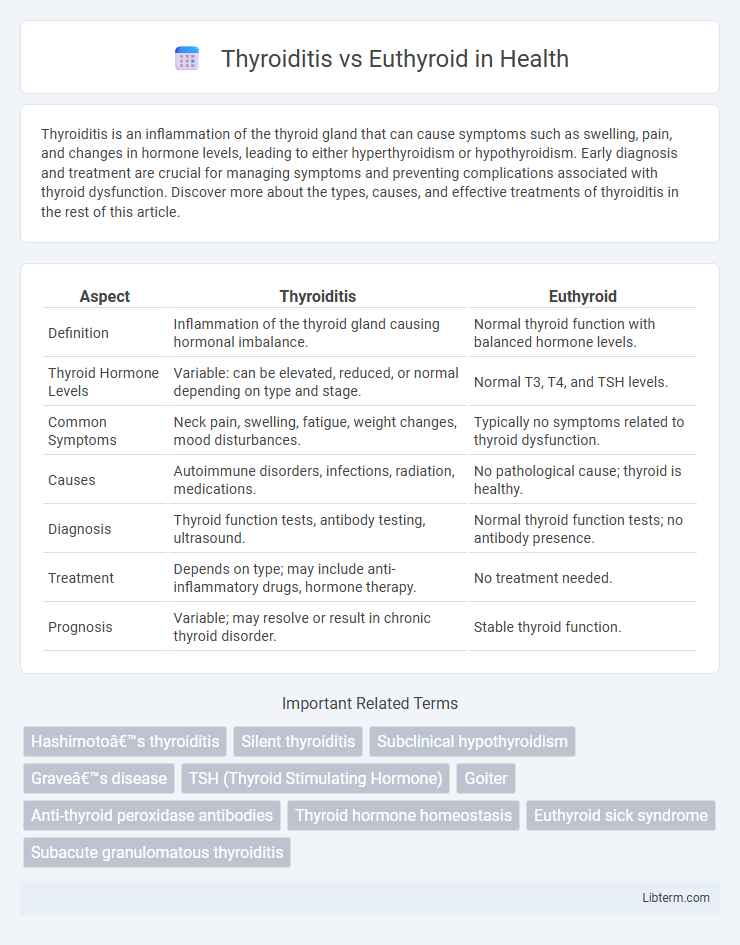
| Aspect | Thyroiditis | Euthyroid |
|---|---|---|
| Definition | Inflammation of the thyroid gland causing hormonal imbalance. | Normal thyroid function with balanced hormone levels. |
| Thyroid Hormone Levels | Variable: can be elevated, reduced, or normal depending on type and stage. | Normal T3, T4, and TSH levels. |
| Common Symptoms | Neck pain, swelling, fatigue, weight changes, mood disturbances. | Typically no symptoms related to thyroid dysfunction. |
| Causes | Autoimmune disorders, infections, radiation, medications. | No pathological cause; thyroid is healthy. |
| Diagnosis | Thyroid function tests, antibody testing, ultrasound. | Normal thyroid function tests; no antibody presence. |
| Treatment | Depends on type; may include anti-inflammatory drugs, hormone therapy. | No treatment needed. |
| Prognosis | Variable; may resolve or result in chronic thyroid disorder. | Stable thyroid function. |
Introduction to Thyroiditis and Euthyroid States
Thyroiditis encompasses a group of inflammatory disorders affecting the thyroid gland, often resulting in transient or permanent alterations in thyroid hormone levels, including hypothyroidism or hyperthyroidism. The euthyroid state refers to normal thyroid function, where circulating thyroid hormone levels--thyroxine (T4) and triiodothyronine (T3)--are within physiological ranges, maintaining metabolic homeostasis. Understanding the distinction between thyroiditis-induced dysfunction and euthyroid status is critical for accurate diagnosis and effective management of thyroid diseases.
Understanding Thyroid Function and Regulation
Thyroiditis is an inflammation of the thyroid gland that can disrupt hormone production, leading to hypo- or hyperthyroidism, while euthyroid refers to a state where the thyroid gland functions normally with balanced thyroid hormone levels, primarily thyroxine (T4) and triiodothyronine (T3). The hypothalamic-pituitary-thyroid (HPT) axis regulates thyroid function through thyroid-stimulating hormone (TSH) secretion, maintaining homeostasis by adjusting hormone synthesis based on the body's metabolic needs. In thyroiditis, this regulatory process is impaired, causing abnormalities in TSH, T3, and T4 levels, whereas euthyroid status signifies an intact and responsive HPT axis ensuring optimal metabolic function.
Causes of Thyroiditis
Thyroiditis primarily results from autoimmune disorders such as Hashimoto's thyroiditis, viral infections like subacute granulomatous thyroiditis, or post-partum immune changes. Unlike euthyroid conditions where thyroid hormone levels remain normal, thyroiditis involves inflammation that disrupts thyroid function, often causing transient hypothyroidism or hyperthyroidism. Common triggers include viral infections, immune system dysregulation, and certain medications that provoke thyroid tissue inflammation.
Euthyroid: Definition and Clinical Significance
Euthyroid refers to the state of having normal thyroid gland function, characterized by balanced levels of thyroid hormones triiodothyronine (T3) and thyroxine (T4), along with a stable thyroid-stimulating hormone (TSH) level. Clinically significant as a baseline reference, euthyroid status indicates the absence of thyroid dysfunction, aiding doctors in distinguishing between thyroiditis, which involves inflammation and often altered hormone levels, and healthy thyroid function. Maintaining euthyroid conditions is crucial for metabolic homeostasis, cardiovascular health, and overall endocrine system stability.
Symptoms: Thyroiditis vs Euthyroid Presentation
Thyroiditis often presents with symptoms such as neck pain, swelling, fatigue, and fluctuating thyroid hormone levels causing hyperthyroid or hypothyroid states. Euthyroid patients exhibit normal thyroid hormone levels and typically lack symptoms related to thyroid dysfunction, maintaining stable metabolism and energy levels. Differentiating thyroiditis from euthyroid status relies on clinical signs, thyroid function tests, and inflammatory markers.
Diagnostic Approaches for Thyroid Disorders
Thyroiditis diagnosis relies on clinical evaluation, elevated inflammatory markers, thyroid function tests showing variable hormone levels, and thyroid ultrasound revealing gland inflammation or hypoechoic areas. In contrast, euthyroid patients have normal thyroid hormone levels and lack inflammation, making diagnosis primarily reliant on routine thyroid function tests to confirm normal gland activity. Fine-needle aspiration biopsy may be used in uncertain cases to distinguish thyroiditis from other thyroid nodules or malignancies.
Laboratory Findings: Differentiating Thyroiditis from Euthyroid
Thyroiditis typically presents with elevated inflammatory markers such as ESR and CRP, coupled with abnormal thyroid function tests showing elevated TSH and decreased free T4 or T3 levels, indicating hypothyroidism or transient thyrotoxicosis. In contrast, euthyroid individuals maintain normal TSH, free T4, and free T3 levels without inflammatory markers elevation, reflecting intact thyroid hormone production and regulation. The presence of thyroid autoantibodies like anti-thyroid peroxidase (anti-TPO) and anti-thyroglobulin antibodies further aids in distinguishing autoimmune thyroiditis from euthyroid status.
Treatment Strategies for Thyroiditis and Euthyroid Conditions
Treatment strategies for thyroiditis often involve anti-inflammatory medications such as NSAIDs or corticosteroids to reduce inflammation, while hormone replacement therapy may be necessary if hypothyroidism develops. In euthyroid conditions, where thyroid function remains normal, active treatment is typically unnecessary, and management focuses on regular monitoring and addressing underlying causes if symptoms arise. Tailoring treatment to the specific type of thyroiditis and thyroid hormone levels is crucial for effective management and preventing complications.
Prognosis and Potential Complications
Thyroiditis, an inflammation of the thyroid gland, often leads to fluctuating thyroid hormone levels, which can result in hypothyroidism or hyperthyroidism, affecting long-term prognosis and increasing risks such as cardiovascular disease and infertility if untreated. Euthyroid status indicates normal thyroid function, generally associated with a stable prognosis and minimal risk of thyroid-related complications. Monitoring thyroid antibody levels can help predict the progression of thyroiditis and the likelihood of transitioning to persistent thyroid dysfunction or euthyroid remission.
Key Takeaways: Thyroiditis vs Euthyroid Management
Thyroiditis management focuses on controlling inflammation and addressing symptoms like hypothyroidism or hyperthyroidism using anti-inflammatory medications, beta-blockers, or thyroid hormone replacement as needed. Euthyroid patients require regular monitoring without active intervention, emphasizing maintaining normal thyroid function through lifestyle and periodic thyroid function tests. Distinguishing between these conditions is crucial because thyroiditis may lead to fluctuating thyroid hormone levels necessitating tailored treatment, while euthyroid status typically indicates stable thyroid activity without medical therapy.
Thyroiditis Infographic
 libterm.com
libterm.com