Virilization refers to the development of male physical characteristics in females or excessive male traits in males, often due to hormonal imbalances or medical conditions. Symptoms may include deepening of the voice, increased body hair, and muscle growth, which can significantly affect one's quality of life. Discover the causes, symptoms, and treatment options to better understand how virilization can impact your health.
Table of Comparison
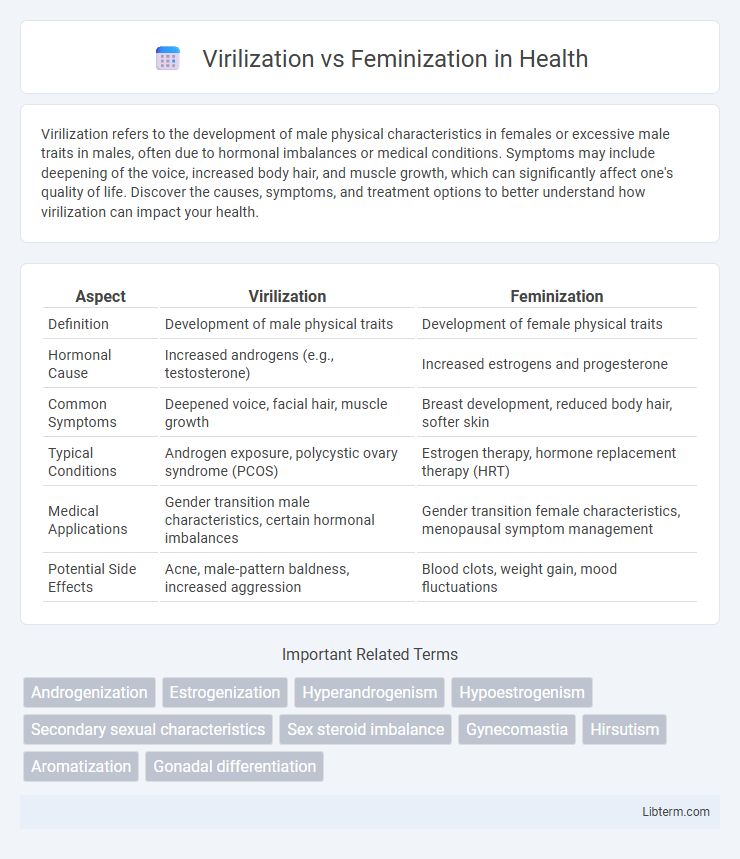
| Aspect | Virilization | Feminization |
|---|---|---|
| Definition | Development of male physical traits | Development of female physical traits |
| Hormonal Cause | Increased androgens (e.g., testosterone) | Increased estrogens and progesterone |
| Common Symptoms | Deepened voice, facial hair, muscle growth | Breast development, reduced body hair, softer skin |
| Typical Conditions | Androgen exposure, polycystic ovary syndrome (PCOS) | Estrogen therapy, hormone replacement therapy (HRT) |
| Medical Applications | Gender transition male characteristics, certain hormonal imbalances | Gender transition female characteristics, menopausal symptom management |
| Potential Side Effects | Acne, male-pattern baldness, increased aggression | Blood clots, weight gain, mood fluctuations |
Understanding Virilization and Feminization
Understanding virilization involves recognizing the development of male physical characteristics such as increased muscle mass, deepening of the voice, and facial hair growth, typically driven by elevated androgen levels. Feminization refers to the process where female secondary sexual characteristics develop, including breast growth, redistribution of body fat, and softer skin, often influenced by higher estrogen levels. Both processes are critical in gender development and hormone therapy, highlighting the importance of hormonal balance in sexual differentiation.
Key Differences Between Virilization and Feminization
Virilization involves the development of male physical characteristics such as increased body hair, deepening of the voice, and muscle growth due to elevated androgen levels, whereas feminization is characterized by the development of female traits including breast growth, fat redistribution, and softer skin linked to higher estrogen levels. Virilization often occurs in females with androgen excess or males undergoing hormonal therapy, while feminization primarily occurs in males receiving estrogen therapy or in conditions like hypogonadism. Key differences lie in hormonal drivers, target physical traits, and clinical contexts, making accurate diagnosis and management critical for addressing underlying endocrine disorders.
Causes of Virilization in Individuals
Virilization in individuals is primarily caused by excessive androgen production from adrenal glands, ovarian tumors, or exogenous androgen use, leading to the development of masculine traits such as deepened voice and increased body hair. Conditions like congenital adrenal hyperplasia (CAH), polycystic ovary syndrome (PCOS), and androgen-secreting tumors disrupt hormonal balance, triggering virilization. Identifying these underlying causes is crucial for targeted treatment and managing symptoms effectively.
Causes of Feminization Processes
Feminization processes are primarily caused by hormonal imbalances, particularly increased levels of estrogen or decreased androgens, which can result from conditions such as liver disease, adrenal tumors, or hormonal therapy. Endocrine disorders like hypogonadism and hyperthyroidism also contribute to feminization by disrupting the normal hormone production and signaling pathways. Certain medications, environmental estrogens, and genetic factors further influence the development of feminization characteristics in individuals.
Hormonal Influences on Virilization and Feminization
Hormonal influences on virilization primarily involve androgens such as testosterone and dihydrotestosterone, which promote the development of male secondary sexual characteristics including increased muscle mass, deepening of the voice, and facial hair growth. Feminization is driven by estrogens and progesterone, which regulate the development of female secondary sexual characteristics such as breast development, fat distribution to hips and thighs, and the regulation of the menstrual cycle. Imbalances or exogenous administration of these hormones can alter typical sexual differentiation and secondary sexual characteristics, leading to conditions of virilization or feminization depending on the dominant hormonal influence.
Clinical Manifestations and Symptoms
Virilization manifests through clinical symptoms such as hirsutism, deepening of the voice, clitoromegaly, and muscle hypertrophy, indicative of excess androgen exposure typically seen in conditions like polycystic ovary syndrome or adrenal hyperplasia. Feminization presents with symptoms including gynecomastia, decreased body hair, and softening of the skin, often associated with increased estrogen levels or androgen deficiency seen in males with hypogonadism or liver cirrhosis. Both conditions involve distinct hormonal imbalances reflected in clinical signs, requiring targeted endocrine evaluation for accurate diagnosis and management.
Diagnostic Methods and Evaluations
Diagnostic methods for virilization and feminization primarily involve hormonal assays, imaging studies, and genetic testing. Evaluations include measuring serum levels of androgens, estrogens, and gonadotropins, alongside pelvic ultrasound or MRI to assess gonadal and adrenal structures. Chromosomal analysis and molecular diagnostics help identify underlying genetic causes contributing to atypical sexual development.
Treatment Options and Management
Treatment options for virilization primarily involve androgen suppression through medications like anti-androgens, GnRH analogs, or corticosteroids, alongside addressing underlying causes such as polycystic ovary syndrome or adrenal hyperplasia. Feminization management often includes hormone replacement therapy with estrogens and anti-androgens to promote secondary female sexual characteristics, coupled with supportive care like psychological counseling and possible surgical interventions for gender confirmation. Both conditions require individualized treatment plans emphasizing hormone levels monitoring, symptom control, and long-term health maintenance to optimize patient outcomes.
Social and Psychological Impacts
Virilization often leads to social challenges such as stigma and discrimination, affecting psychological well-being by causing anxiety and identity conflicts. Feminization may impact social interactions through shifts in gender expectations, potentially resulting in empowerment or social isolation depending on the cultural context. Both processes influence self-esteem and mental health, highlighting the importance of supportive environments and counseling.
Prevention and Long-term Considerations
Preventing virilization and feminization involves hormonal regulation through medical interventions such as hormone replacement therapy (HRT) tailored to individual needs, alongside lifestyle modifications to support endogenous hormone balance. Long-term considerations include monitoring metabolic health, bone density, and psychological well-being to mitigate complications associated with prolonged hormone exposure. Regular endocrinological assessments and personalized care plans are essential to optimize outcomes and prevent irreversible physical changes.
Virilization Infographic
 libterm.com
libterm.com