Osteomalacia and hyperparathyroidism are disorders that significantly affect bone health by disrupting calcium and phosphate balance. Osteomalacia results in soft, weakened bones due to inadequate bone mineralization, often linked to vitamin D deficiency, while hyperparathyroidism causes excessive parathyroid hormone production leading to bone resorption and increased fracture risk. Explore the rest of this article to understand their causes, symptoms, and effective treatment options for maintaining your bone health.
Table of Comparison
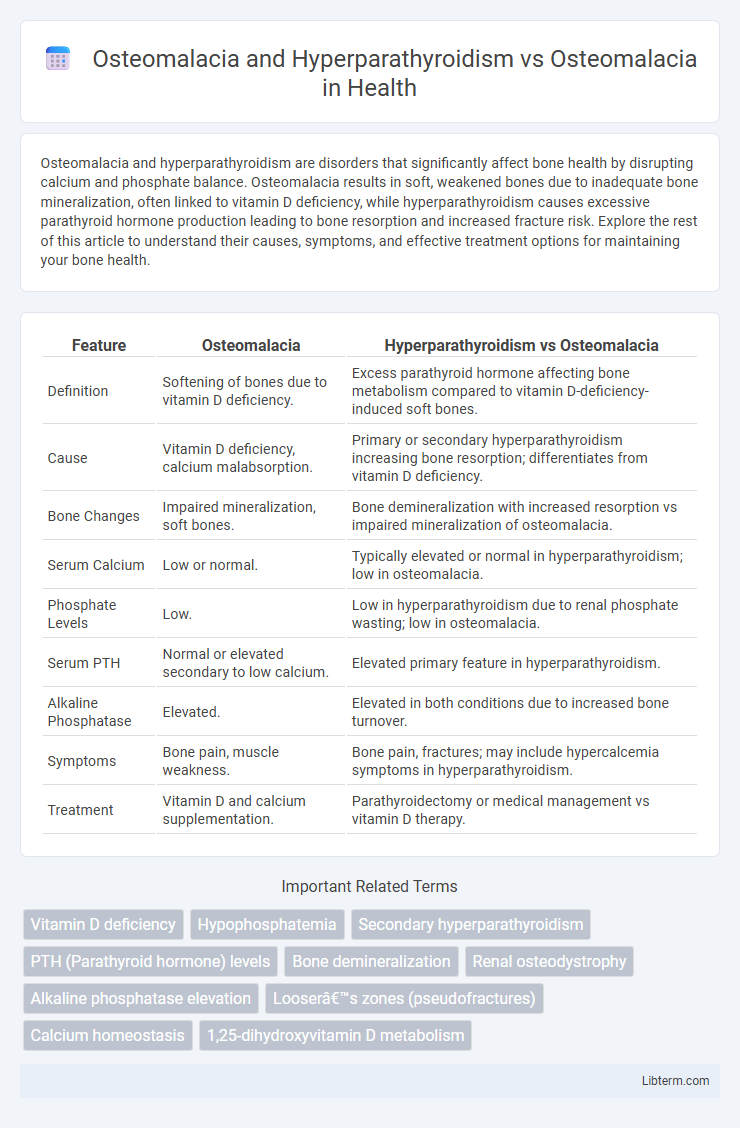
| Feature | Osteomalacia | Hyperparathyroidism vs Osteomalacia |
|---|---|---|
| Definition | Softening of bones due to vitamin D deficiency. | Excess parathyroid hormone affecting bone metabolism compared to vitamin D-deficiency-induced soft bones. |
| Cause | Vitamin D deficiency, calcium malabsorption. | Primary or secondary hyperparathyroidism increasing bone resorption; differentiates from vitamin D deficiency. |
| Bone Changes | Impaired mineralization, soft bones. | Bone demineralization with increased resorption vs impaired mineralization of osteomalacia. |
| Serum Calcium | Low or normal. | Typically elevated or normal in hyperparathyroidism; low in osteomalacia. |
| Phosphate Levels | Low. | Low in hyperparathyroidism due to renal phosphate wasting; low in osteomalacia. |
| Serum PTH | Normal or elevated secondary to low calcium. | Elevated primary feature in hyperparathyroidism. |
| Alkaline Phosphatase | Elevated. | Elevated in both conditions due to increased bone turnover. |
| Symptoms | Bone pain, muscle weakness. | Bone pain, fractures; may include hypercalcemia symptoms in hyperparathyroidism. |
| Treatment | Vitamin D and calcium supplementation. | Parathyroidectomy or medical management vs vitamin D therapy. |
Understanding Osteomalacia: Definition and Causes
Osteomalacia is a metabolic bone disorder characterized by defective bone mineralization, leading to soft and weakened bones primarily due to vitamin D deficiency or impaired phosphate metabolism. In contrast, osteomalacia associated with hyperparathyroidism involves excessive parathyroid hormone secretion, which disrupts calcium and phosphate balance, exacerbating bone demineralization. Understanding these distinctions clarifies that while classic osteomalacia results mainly from nutritional or metabolic deficiencies, hyperparathyroidism-induced osteomalacia stems from endocrine dysregulation affecting bone remodeling.
What is Hyperparathyroidism? Key Features and Mechanisms
Hyperparathyroidism is a disorder characterized by excessive secretion of parathyroid hormone (PTH), leading to abnormal calcium and phosphate metabolism. Key features include hypercalcemia, bone resorption, kidney stones, and neuromuscular symptoms resulting from increased osteoclastic activity and calcium release from bones. The underlying mechanism involves overstimulation of PTH receptors, causing increased calcium reabsorption in kidneys, enhanced intestinal calcium absorption via activated vitamin D, and bone demineralization, which differentiates it from osteomalacia that primarily involves defective bone mineralization due to vitamin D deficiency.
Osteomalacia vs. Hyperparathyroidism: Pathophysiological Differences
Osteomalacia is characterized by defective bone mineralization due to vitamin D deficiency, leading to soft, weak bones, whereas hyperparathyroidism involves excessive parathyroid hormone secretion causing increased bone resorption and calcium mobilization from bone. In osteomalacia, impaired calcium and phosphate incorporation into the bone matrix results in accumulation of unmineralized osteoid, while hyperparathyroidism stimulates osteoclast activity, promoting bone demineralization and potential osteoporosis. The distinct pathophysiological mechanisms reflect contrasting biochemical profiles: low serum calcium and phosphate in osteomalacia versus hypercalcemia and hypophosphatemia in hyperparathyroidism.
Clinical Manifestations: Comparing Symptoms
Osteomalacia presents with bone pain, muscle weakness, and difficulty walking due to defective bone mineralization, while hyperparathyroidism causes bone resorption, leading to bone pain, fractures, and skeletal deformities. Both conditions exhibit bone tenderness and fractures, but hyperparathyroidism may also show symptoms of hypercalcemia, such as kidney stones and gastrointestinal disturbances. Differentiating clinical manifestations relies on assessing biochemical markers, including serum calcium, phosphate, alkaline phosphatase, and parathyroid hormone levels.
Biochemical Markers: Diagnostic Laboratory Differences
Osteomalacia presents with low serum calcium, decreased phosphate levels, elevated alkaline phosphatase, and low or normal parathyroid hormone (PTH). In contrast, osteomalacia with secondary hyperparathyroidism shows elevated PTH due to hypocalcemia or phosphate imbalance, often accompanied by decreased serum calcium and phosphate and increased alkaline phosphatase. Distinguishing these biochemical markers is crucial for accurate diagnosis and targeted treatment strategies.
Radiological Findings: Imaging Insights
Radiological findings in osteomalacia typically reveal Looser's zones, characterized by pseudofractures predominantly in the femoral neck and ribs, along with generalized osteopenia. In hyperparathyroidism-associated osteomalacia, imaging shows subperiosteal bone resorption, especially along the radial aspects of the middle phalanges, salt-and-pepper skull appearance, and brown tumors, combined with osteomalacic features such as Looser's zones. Differentiating these conditions radiologically hinges on identifying hyperparathyroid-specific bone changes superimposed on the characteristic osteomalacia radiographic spectrum.
Risk Factors for Osteomalacia and Hyperparathyroidism
Risk factors for osteomalacia and hyperparathyroidism include vitamin D deficiency, chronic kidney disease, and malabsorption syndromes, which impair calcium and phosphate metabolism essential for bone mineralization. In hyperparathyroidism, excessive parathyroid hormone secretion leads to increased bone resorption and subsequent osteomalacia, especially when coupled with nutritional deficiencies or renal dysfunction. Genetic predispositions, certain medications, and lack of sunlight exposure further elevate the risk of developing these intertwined metabolic bone disorders.
Treatment Approaches: Osteomalacia vs. Hyperparathyroidism
Treatment of osteomalacia primarily involves vitamin D and calcium supplementation to correct mineral deficiencies and improve bone mineralization. In hyperparathyroidism-induced osteomalacia, addressing the underlying parathyroid hormone imbalance through surgical removal of parathyroid adenomas or pharmacological agents like calcimimetics is crucial alongside correcting bone demineralization. Management strategies diverge significantly as osteomalacia focuses on nutrient replenishment, while hyperparathyroidism requires targeted hormone regulation to prevent further bone resorption.
Prognosis and Long-Term Outcomes
Osteomalacia caused by vitamin D deficiency generally has a favorable prognosis with proper supplementation and correction of underlying causes, leading to reversal of bone pain and improved mineralization. In contrast, osteomalacia secondary to hyperparathyroidism presents a more complex long-term outcome due to persistent elevated parathyroid hormone levels causing continuous bone resorption and increased fracture risk. Effective management of hyperparathyroidism is critical to improving prognosis by normalizing calcium and phosphate metabolism, thereby reducing skeletal complications associated with osteomalacia in these patients.
Preventive Strategies and Patient Education
Preventive strategies for osteomalacia focus on ensuring adequate vitamin D and calcium intake through diet and supplements, along with regular sunlight exposure to enhance vitamin D synthesis. In cases where osteomalacia coexists with hyperparathyroidism, managing parathyroid hormone levels through medical treatment or surgery is essential to prevent further bone demineralization. Patient education should emphasize the importance of nutritional compliance, monitoring biochemical markers like serum calcium and alkaline phosphatase, and recognizing symptoms of bone pain or muscle weakness for timely intervention.
Osteomalacia and Hyperparathyroidism Infographic
 libterm.com
libterm.com