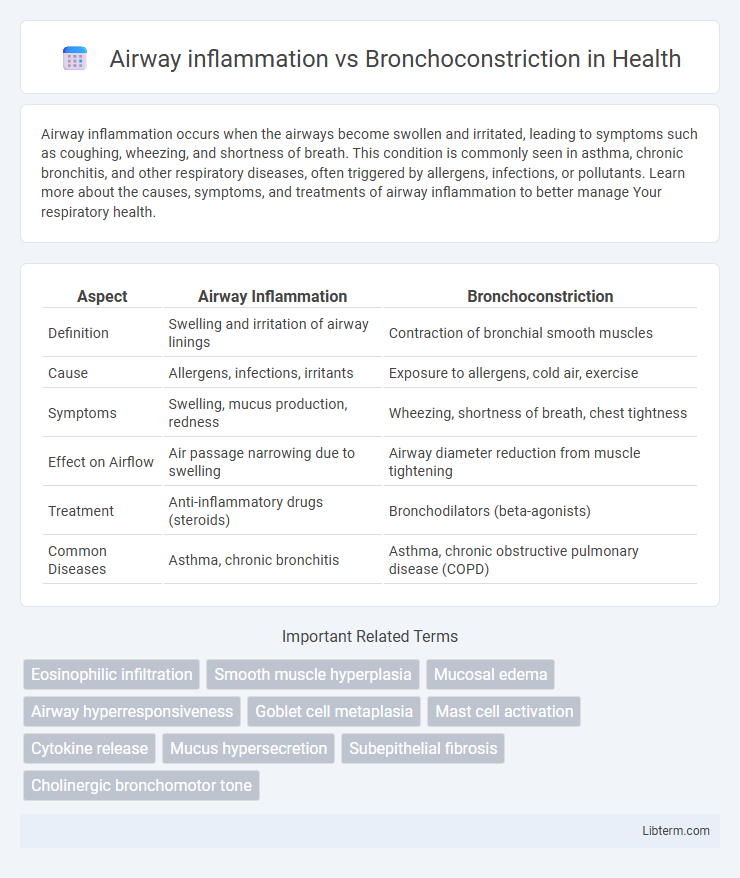
Airway inflammation occurs when the airways become swollen and irritated, leading to symptoms such as coughing, wheezing, and shortness of breath. This condition is commonly seen in asthma, chronic bronchitis, and other respiratory diseases, often triggered by allergens, infections, or pollutants. Learn more about the causes, symptoms, and treatments of airway inflammation to better manage Your respiratory health.
Table of Comparison
| Aspect | Airway Inflammation | Bronchoconstriction |
|---|---|---|
| Definition | Swelling and irritation of airway linings | Contraction of bronchial smooth muscles |
| Cause | Allergens, infections, irritants | Exposure to allergens, cold air, exercise |
| Symptoms | Swelling, mucus production, redness | Wheezing, shortness of breath, chest tightness |
| Effect on Airflow | Air passage narrowing due to swelling | Airway diameter reduction from muscle tightening |
| Treatment | Anti-inflammatory drugs (steroids) | Bronchodilators (beta-agonists) |
| Common Diseases | Asthma, chronic bronchitis | Asthma, chronic obstructive pulmonary disease (COPD) |
Understanding Airway Inflammation: Definition and Mechanisms
Airway inflammation involves the immune system's response to irritants or allergens, leading to swelling, increased mucus production, and infiltration of inflammatory cells such as eosinophils and neutrophils. This process causes structural changes in the airway walls, contributing to hyperresponsiveness and chronic respiratory conditions like asthma and chronic obstructive pulmonary disease (COPD). Understanding the molecular mediators, including cytokines and chemokines, is crucial for targeting inflammation and preventing airway obstruction and bronchoconstriction.
What is Bronchoconstriction? Causes and Processes
Bronchoconstriction is the narrowing of the airways in the lungs due to the tightening of surrounding smooth muscle, leading to restricted airflow and difficulty breathing. It is commonly triggered by asthma, allergic reactions, exposure to irritants such as smoke or pollutants, respiratory infections, and exercise-induced bronchospasm. The process involves the release of inflammatory mediators like histamine and leukotrienes, which stimulate muscle contraction and mucus production, further obstructing the bronchial passages.
Key Differences Between Airway Inflammation and Bronchoconstriction
Airway inflammation involves swelling and irritation of the bronchial tubes, leading to mucus production and tissue damage, while bronchoconstriction refers to the tightening of the muscles surrounding the airways, causing narrowed air passages. Inflammatory markers such as eosinophils and cytokines are elevated during airway inflammation, whereas bronchoconstriction primarily results from smooth muscle contraction triggered by stimuli like allergens or irritants. Effective asthma management requires distinguishing between these processes, as anti-inflammatory medications target airway inflammation, and bronchodilators relieve bronchoconstriction.
Triggers and Risk Factors for Airway Inflammation
Airway inflammation is primarily triggered by allergens such as pollen, dust mites, and pet dander, as well as irritants like tobacco smoke, pollution, and respiratory infections. Risk factors for airway inflammation include genetic predisposition to asthma, exposure to environmental pollutants, and a history of atopic diseases such as eczema or allergic rhinitis. In contrast, bronchoconstriction is usually a response to these inflammatory triggers, resulting in the tightening of airway smooth muscles and airflow limitation.
Common Triggers of Bronchoconstriction
Common triggers of bronchoconstriction include allergens like pollen, dust mites, and pet dander, respiratory infections, cold air exposure, exercise, and irritants such as tobacco smoke and chemical fumes. Bronchoconstriction results from the tightening of airway smooth muscles, leading to narrowed airways and difficulty breathing. Unlike airway inflammation, which involves swelling and mucus production, bronchoconstriction primarily involves the constriction of bronchial muscles triggered by these environmental and physiological factors.
Symptoms: Airway Inflammation vs Bronchoconstriction
Airway inflammation typically causes symptoms such as persistent cough, wheezing, and shortness of breath due to swelling and mucus buildup in the airways. Bronchoconstriction primarily results in tightness in the chest, rapid breathing, and difficulty exhaling caused by the narrowing of bronchial muscles. Differentiating these symptoms helps target treatment approaches for conditions like asthma and chronic bronchitis.
Diagnostic Approaches: Identifying Airway Inflammation and Bronchoconstriction
Diagnostic approaches for airway inflammation include sputum analysis, exhaled nitric oxide measurement (FeNO), and imaging techniques like high-resolution CT scans to detect mucosal edema and cellular infiltration. Bronchoconstriction is primarily assessed through spirometry with bronchodilator response testing and methacholine challenge tests, revealing reversible airway obstruction and hyperresponsiveness. Combining inflammatory biomarkers with functional respiratory tests provides a comprehensive evaluation distinguishing airway inflammation from bronchoconstriction in respiratory diseases.
Treatment Strategies for Airway Inflammation
Treatment strategies for airway inflammation primarily involve the use of anti-inflammatory medications such as inhaled corticosteroids, leukotriene modifiers, and biologics targeting specific inflammatory pathways. These therapies aim to reduce airway edema, mucus production, and immune cell infiltration, thereby preventing long-term airway remodeling and improving lung function. Unlike bronchoconstriction treatments that focus on bronchodilators like beta-agonists, managing airway inflammation requires sustained control of the underlying inflammatory process to achieve optimal respiratory outcomes.
Managing and Relieving Bronchoconstriction
Managing bronchoconstriction involves the use of bronchodilators such as short-acting beta-agonists (SABAs) to quickly relax airway smooth muscles and improve airflow during asthma attacks. Anti-inflammatory medications like inhaled corticosteroids are essential to reduce airway inflammation, preventing the frequency and severity of bronchoconstriction episodes. Proper management combines these therapies to control symptoms, improve lung function, and enhance patient quality of life.
Prevention and Long-Term Management of Airway Disorders
Effective long-term management of airway disorders prioritizes reducing airway inflammation through regular use of inhaled corticosteroids and avoiding environmental triggers such as allergens and smoke. Bronchoconstriction is controlled by bronchodilators like beta-agonists, which provide rapid relief but do not address underlying inflammation. Preventing airway inflammation minimizes the frequency and severity of bronchoconstriction episodes, thereby improving overall respiratory function and reducing hospitalizations.
Airway inflammation Infographic
 libterm.com
libterm.com