Pathogenicity refers to the ability of a microorganism to cause disease in a host organism, determined by factors such as virulence, infection mechanisms, and immune evasion strategies. Understanding these mechanisms helps in developing effective treatments and preventive measures against infectious diseases. Dive deeper into the article to explore how pathogenicity impacts health and disease management.
Table of Comparison
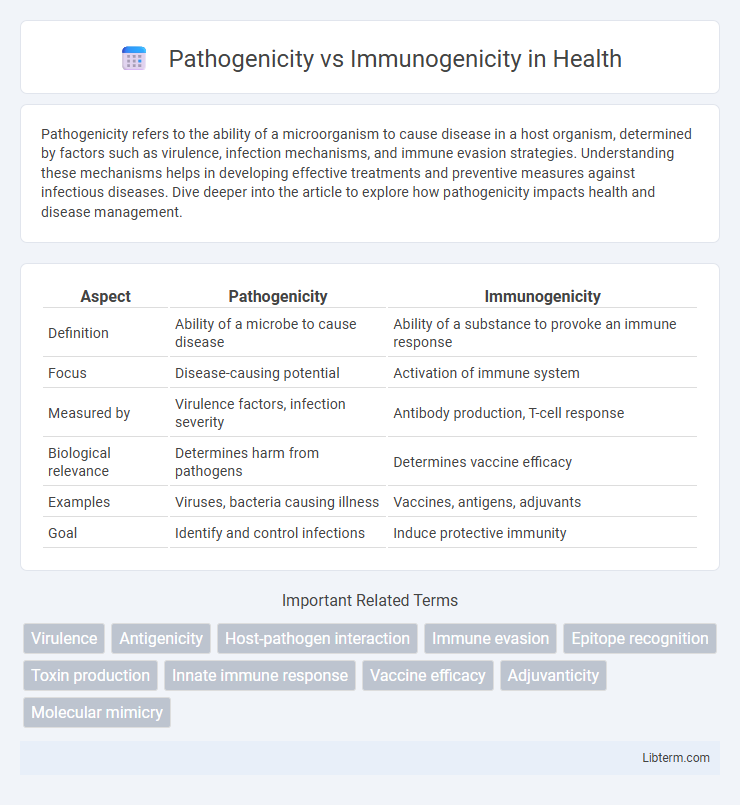
| Aspect | Pathogenicity | Immunogenicity |
|---|---|---|
| Definition | Ability of a microbe to cause disease | Ability of a substance to provoke an immune response |
| Focus | Disease-causing potential | Activation of immune system |
| Measured by | Virulence factors, infection severity | Antibody production, T-cell response |
| Biological relevance | Determines harm from pathogens | Determines vaccine efficacy |
| Examples | Viruses, bacteria causing illness | Vaccines, antigens, adjuvants |
| Goal | Identify and control infections | Induce protective immunity |
Introduction to Pathogenicity and Immunogenicity
Pathogenicity refers to a microorganism's ability to cause disease in a host by overcoming immune defenses and causing tissue damage. Immunogenicity describes the capacity of a substance, such as an antigen or vaccine, to provoke an immune response, including antibody production and cellular immunity. Understanding the balance between pathogenicity and immunogenicity is essential for developing effective vaccines and therapeutic interventions.
Defining Pathogenicity: What Makes an Organism Harmful?
Pathogenicity refers to an organism's ability to cause disease by invading host tissues, evading immune defenses, and producing toxins that disrupt normal physiological functions. Factors determining pathogenicity include virulence factors such as adhesins, invasins, and enzymes that facilitate colonization and damage. Understanding the molecular mechanisms behind pathogenicity helps differentiate harmful pathogens from non-pathogenic microbes by their capacity to induce host pathology.
Understanding Immunogenicity: How the Immune System Responds
Immunogenicity refers to the ability of a substance, such as an antigen or vaccine, to provoke an immune response by activating immune cells like B and T lymphocytes. The immune system recognizes specific epitopes on pathogens or foreign molecules, triggering antibody production and memory cell formation for long-term protection. Unlike pathogenicity, which describes a microorganism's capacity to cause disease, immunogenicity emphasizes the interaction between antigens and the host immune system, critical for vaccine efficacy and immune defense.
Key Differences Between Pathogenicity and Immunogenicity
Pathogenicity refers to the ability of a microorganism to cause disease, while immunogenicity measures the capacity of a pathogen or antigen to provoke an immune response in the host. Pathogenicity involves factors like virulence determinants and host susceptibility, whereas immunogenicity depends on antigen recognition, immune cell activation, and memory formation. Key differences include pathogenicity leading directly to disease symptoms, whereas immunogenicity results in protective immunity without necessarily causing illness.
Factors Influencing Pathogenicity
Factors influencing pathogenicity include the microorganism's ability to adhere to host cells, invade tissues, and evade the host immune response through mechanisms such as antigenic variation and secretion of immunosuppressive molecules. Virulence factors like toxins, enzymes, and capsules enhance pathogenic potential by damaging host tissues and interfering with immune functions. Environmental conditions, host susceptibility, and microbial load also critically determine the degree of pathogenicity expressed during infection.
Factors Affecting Immunogenicity
Factors affecting immunogenicity include the molecular size, with larger molecules typically eliciting stronger immune responses, and chemical complexity, where proteins and polysaccharides are more immunogenic than lipids or nucleic acids. The route of antigen administration significantly influences immunogenicity; for instance, intradermal injection often produces a more potent immune response compared to oral or intravenous routes. Host-related factors such as genetic background, age, and immune status also play crucial roles in determining the strength and nature of the immune response to an antigen.
Examples of Pathogenic and Immunogenic Agents
Pathogenic agents such as Mycobacterium tuberculosis and Influenza virus cause disease by invading and damaging host tissues, leading to clinical symptoms. Immunogenic agents like the Hepatitis B surface antigen and tetanus toxoid stimulate a strong immune response without causing disease, making them effective components in vaccines. Understanding the distinction between pathogenicity and immunogenicity helps in developing targeted therapies and preventive measures against infectious diseases.
Clinical Significance: Pathogenicity in Disease Progression
Pathogenicity refers to the ability of a microorganism to cause disease by invading host tissues, evading the immune system, and producing toxins or damaging factors that trigger clinical symptoms. Immunogenicity describes the capacity of an antigen to provoke an immune response, which can influence the severity and outcome of infections by controlling or eliminating pathogens. In clinical settings, high pathogenicity often correlates with severe disease progression and complications, whereas strong immunogenicity is crucial for effective vaccine development and immune-mediated clearance of infectious agents.
Immunogenicity in Vaccine Development
Immunogenicity is the ability of a substance, such as a vaccine antigen, to provoke an immune response, which is critical for effective vaccine development. Measuring immunogenicity involves assessing antibody production, T-cell activation, and memory cell formation to ensure lasting protection against pathogens. Optimizing immunogenicity in vaccines enhances safety, efficacy, and durability of immune protection, making it a key focus in preventing infectious diseases.
Implications for Disease Prevention and Treatment
Understanding the distinction between pathogenicity and immunogenicity is crucial for developing effective disease prevention and treatment strategies. Pathogenicity refers to a microbe's ability to cause disease, while immunogenicity denotes its capacity to induce an immune response. Targeting immunogenic components in vaccines enhances protective immunity, whereas recognizing pathogenic traits aids in diagnosing infection severity and tailoring antimicrobial therapies.
Pathogenicity Infographic
 libterm.com
libterm.com