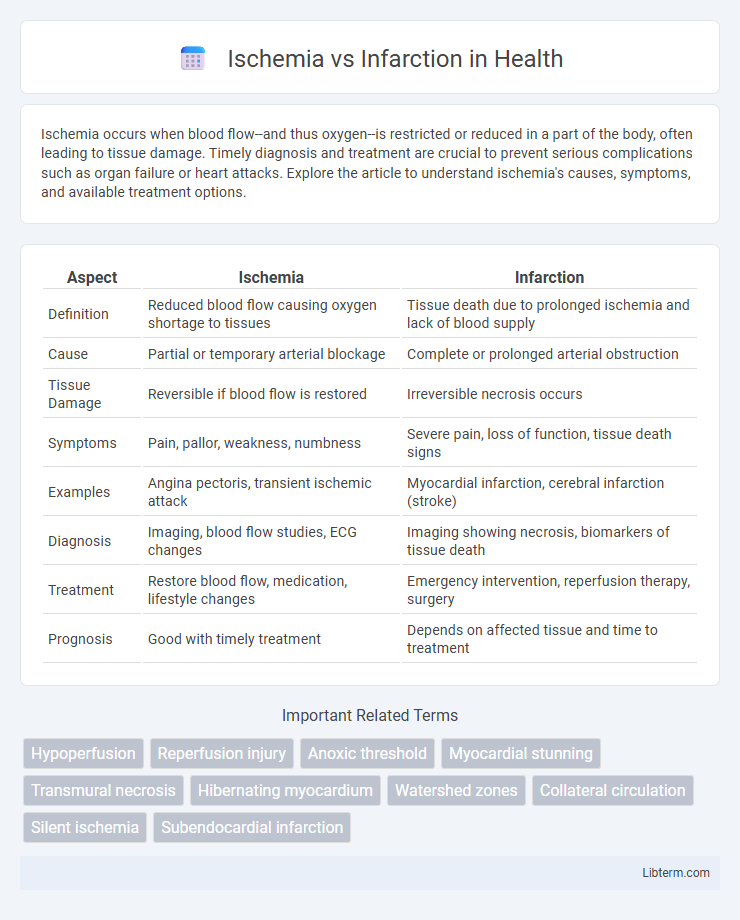
Ischemia occurs when blood flow--and thus oxygen--is restricted or reduced in a part of the body, often leading to tissue damage. Timely diagnosis and treatment are crucial to prevent serious complications such as organ failure or heart attacks. Explore the article to understand ischemia's causes, symptoms, and available treatment options.
Table of Comparison
| Aspect | Ischemia | Infarction |
|---|---|---|
| Definition | Reduced blood flow causing oxygen shortage to tissues | Tissue death due to prolonged ischemia and lack of blood supply |
| Cause | Partial or temporary arterial blockage | Complete or prolonged arterial obstruction |
| Tissue Damage | Reversible if blood flow is restored | Irreversible necrosis occurs |
| Symptoms | Pain, pallor, weakness, numbness | Severe pain, loss of function, tissue death signs |
| Examples | Angina pectoris, transient ischemic attack | Myocardial infarction, cerebral infarction (stroke) |
| Diagnosis | Imaging, blood flow studies, ECG changes | Imaging showing necrosis, biomarkers of tissue death |
| Treatment | Restore blood flow, medication, lifestyle changes | Emergency intervention, reperfusion therapy, surgery |
| Prognosis | Good with timely treatment | Depends on affected tissue and time to treatment |
Understanding Ischemia and Infarction
Ischemia refers to the reduced blood flow to tissues, causing a shortage of oxygen and nutrients essential for cellular metabolism, which can lead to reversible tissue damage if promptly resolved. Infarction occurs when ischemia persists long enough to cause irreversible cell death, resulting in tissue necrosis, commonly seen in myocardial infarction or stroke. Understanding ischemia and infarction is critical for early diagnosis and intervention to prevent permanent organ damage.
Key Differences Between Ischemia and Infarction
Ischemia refers to the reduction of blood flow to tissues, causing oxygen deprivation without immediate cell death, whereas infarction involves irreversible tissue necrosis due to prolonged ischemia. The key difference lies in the severity and outcome; ischemia can be reversible if treated promptly, while infarction results in permanent damage. Clinically, infarction is often identified by specific markers such as elevated troponin in myocardial infarction, distinguishing it from transient ischemic episodes.
Causes of Ischemia
Ischemia occurs when blood flow to a tissue is reduced, primarily caused by atherosclerosis, thrombosis, or arterial embolism that narrows or blocks arteries. Other causes include vasospasm, low blood pressure (hypotension), and external compression of blood vessels. These factors lead to insufficient oxygen delivery, increasing the risk of tissue damage or infarction if the ischemia persists.
Causes of Infarction
Infarction results from prolonged ischemia, where insufficient blood flow causes irreversible tissue death, primarily due to arterial occlusion by thrombosis or embolism. Common causes include atherosclerosis leading to coronary artery blockage, emboli originating from cardiac sources like atrial fibrillation, and vasospasm reducing blood supply. Understanding these etiologies is crucial for accurate diagnosis and targeted treatment to prevent further tissue damage.
Pathophysiology: How Ischemia Develops
Ischemia develops when blood flow restriction causes insufficient oxygen delivery to tissues, leading to a shift from aerobic to anaerobic metabolism and accumulation of lactic acid. This metabolic disturbance results in cellular energy depletion, ion pump failure, and cellular swelling. Prolonged ischemia triggers irreversible cell injury, progressing to infarction characterized by tissue necrosis.
Pathophysiology: How Infarction Occurs
Infarction occurs when prolonged ischemia causes irreversible tissue necrosis due to sustained oxygen and nutrient deprivation. The pathophysiological process begins with arterial occlusion or severe blood flow reduction, leading to cellular hypoxia, depletion of ATP, and failure of ion pumps. Resulting cellular swelling, membrane rupture, and release of enzymes trigger inflammation and further tissue damage, solidifying the infarcted area.
Clinical Signs and Symptoms
Ischemia presents with transient symptoms such as chest pain, pallor, and diaphoresis due to reduced blood flow causing tissue oxygen deprivation. Infarction manifests more severely with persistent chest pain, localized tenderness, and signs of tissue necrosis including elevated cardiac enzymes and ECG changes. Recognizing the severity and duration of these clinical signs aids in differentiating ischemia from infarction in diagnostic evaluation.
Diagnostic Approaches
Diagnostic approaches for ischemia primarily involve stress testing combined with electrocardiography (ECG) or imaging techniques like nuclear scintigraphy, echocardiography, and cardiac MRI to detect reversible myocardial perfusion defects. Infarction diagnosis emphasizes biomarker analysis, including elevated troponin levels, alongside ECG changes such as ST-segment elevation or Q waves, and confirmatory imaging modalities like cardiac MRI or computed tomography to identify permanent myocardial damage. Coronary angiography remains crucial in both conditions for assessing the extent of coronary artery obstruction and guiding interventional strategies.
Treatment and Management Options
Ischemia treatment primarily involves restoring blood flow through medications like antiplatelets and vasodilators, along with lifestyle modifications to reduce cardiovascular risk factors. Infarction management requires urgent revascularization procedures such as percutaneous coronary intervention (PCI) or thrombolytic therapy to limit tissue damage, combined with supportive care including pain control and hemodynamic stabilization. Long-term strategies for both conditions emphasize secondary prevention using beta-blockers, ACE inhibitors, statins, and cardiac rehabilitation to improve outcomes and reduce recurrence.
Preventive Measures and Prognosis
Ischemia prevention primarily involves managing risk factors such as hypertension, diabetes, smoking cessation, and maintaining a healthy diet to improve blood flow and reduce arterial blockage. Early intervention in ischemia can prevent progression to infarction, which is tissue death due to prolonged lack of blood supply, significantly worsening prognosis. Prognosis depends on timely restoration of circulation; infarction often results in permanent tissue damage and higher risk of complications like heart failure or stroke, emphasizing the importance of rapid treatment and lifestyle modifications.
Ischemia Infographic
 libterm.com
libterm.com