Complications can arise unexpectedly during medical treatment, impacting recovery and overall health outcomes. Understanding potential risks and early signs is crucial for prompt intervention and minimizing long-term effects. Explore the rest of this article to learn how to recognize and manage complications effectively.
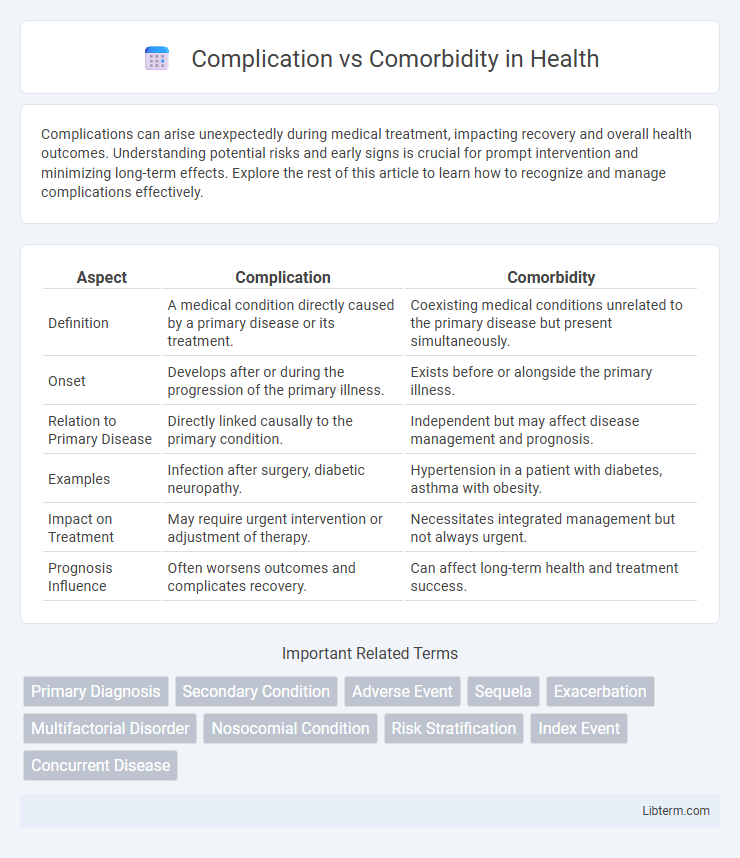
Table of Comparison
| Aspect | Complication | Comorbidity |
|---|---|---|
| Definition | A medical condition directly caused by a primary disease or its treatment. | Coexisting medical conditions unrelated to the primary disease but present simultaneously. |
| Onset | Develops after or during the progression of the primary illness. | Exists before or alongside the primary illness. |
| Relation to Primary Disease | Directly linked causally to the primary condition. | Independent but may affect disease management and prognosis. |
| Examples | Infection after surgery, diabetic neuropathy. | Hypertension in a patient with diabetes, asthma with obesity. |
| Impact on Treatment | May require urgent intervention or adjustment of therapy. | Necessitates integrated management but not always urgent. |
| Prognosis Influence | Often worsens outcomes and complicates recovery. | Can affect long-term health and treatment success. |
Understanding Complications: Definition and Examples
Complications are adverse conditions that arise directly as a result of a primary disease or its treatment, such as infection developing after surgery or heart failure following a myocardial infarction. They represent a worsening or extension of the initial health issue, often requiring immediate medical intervention to prevent further deterioration. Examples include pneumonia as a complication of influenza or diabetic ketoacidosis as a complication of poorly controlled diabetes.
What Are Comorbidities? Key Concepts Explained
Comorbidities refer to the presence of one or more additional diseases or disorders co-occurring with a primary condition, significantly impacting patient management and outcomes. These conditions can interact synergistically or independently, complicating diagnosis, treatment, and prognosis. Understanding comorbidities is crucial for comprehensive healthcare, as they influence disease progression, therapeutic decisions, and overall patient quality of life.
Complication vs Comorbidity: Core Differences
Complications refer to new problems that arise during the course of a disease, often worsening the patient's condition or prolonging recovery, while comorbidities are existing, independent health conditions that coexist with the primary disease. The core difference lies in causality; complications develop as a direct or indirect result of the primary illness or its treatment, whereas comorbidities are separate diseases that may influence overall prognosis but are not caused by the primary disease. Understanding this distinction is crucial for accurate diagnosis, treatment planning, and patient management in clinical practice.
Clinical Impact of Complications in Patient Care
Complications in patient care significantly worsen clinical outcomes by introducing new health problems that prolong hospitalization, increase treatment complexity, and elevate mortality risk. Unlike comorbidities, which are pre-existing conditions present at admission, complications arise due to disease progression or medical interventions, directly impacting recovery trajectories. Effective management of complications is crucial to reduce healthcare costs, prevent functional decline, and improve overall patient prognosis.
The Role of Comorbidities in Disease Progression
Comorbidities significantly influence disease progression by exacerbating symptoms and complicating treatment outcomes, often leading to increased morbidity and mortality rates. The presence of additional chronic conditions, such as diabetes or hypertension alongside a primary illness, can alter the disease's natural course and limit therapeutic options. Understanding the interplay between comorbidities and primary diseases is essential for developing tailored clinical management strategies and improving patient prognosis.
Diagnosing Complications: Criteria and Methods
Diagnosing complications involves identifying new conditions that arise directly from a primary disease or its treatment, often requiring specific clinical criteria and diagnostic tests to distinguish them from pre-existing comorbidities. Methods include thorough patient history evaluation, targeted laboratory tests, and imaging studies to detect deviations indicating disease progression or adverse effects. Accurate differentiation between complications and comorbidities is crucial for effective treatment planning and improved patient outcomes.
Identification and Management of Comorbid Conditions
Identification of comorbid conditions involves comprehensive patient history review, diagnostic testing, and use of standardized assessment tools to detect concurrent diseases that impact primary illness management. Effective management requires integrated care plans, multidisciplinary collaboration, and individualized treatment strategies targeting both the primary condition and comorbidities to improve overall patient outcomes. Regular monitoring and adjustment of therapies help prevent complications and optimize disease control across all identified comorbidities.
How Complications Affect Treatment Outcomes
Complications, defined as new medical problems arising during treatment, significantly worsen treatment outcomes by prolonging recovery times and increasing healthcare costs. Unlike comorbidities, which are pre-existing conditions, complications directly result from the primary illness or its intervention, often leading to increased morbidity and mortality rates. Effective management of complications is critical to improving patient prognosis and ensuring successful therapeutic results.
Comorbidities and Their Influence on Prognosis
Comorbidities significantly impact prognosis by exacerbating the primary disease course and complicating treatment strategies. The presence of multiple chronic conditions, such as diabetes, hypertension, or chronic obstructive pulmonary disease, often leads to increased mortality rates and prolonged hospital stays. Effective management of comorbidities is essential for improving patient outcomes and reducing healthcare costs.
Strategies for Managing Complications and Comorbidities
Effective strategies for managing complications and comorbidities involve early detection through comprehensive diagnostic evaluations and continuous monitoring of patient health status. Personalized treatment plans that integrate multidisciplinary approaches--combining pharmacological therapies, lifestyle modifications, and patient education--are essential for improving outcomes. Coordination among healthcare providers and the use of advanced health information systems facilitate timely interventions and reduce the risk of adverse events.
Complication Infographic
 libterm.com
libterm.com