Gout and rheumatoid arthritis are both forms of arthritis that cause joint pain and inflammation but differ significantly in their causes and treatment approaches. Gout results from the buildup of uric acid crystals in the joints, often leading to sudden, intense pain, while rheumatoid arthritis is an autoimmune disorder that causes chronic inflammation and joint damage. Explore the rest of the article to understand how to differentiate and manage these conditions effectively for your health.
Table of Comparison
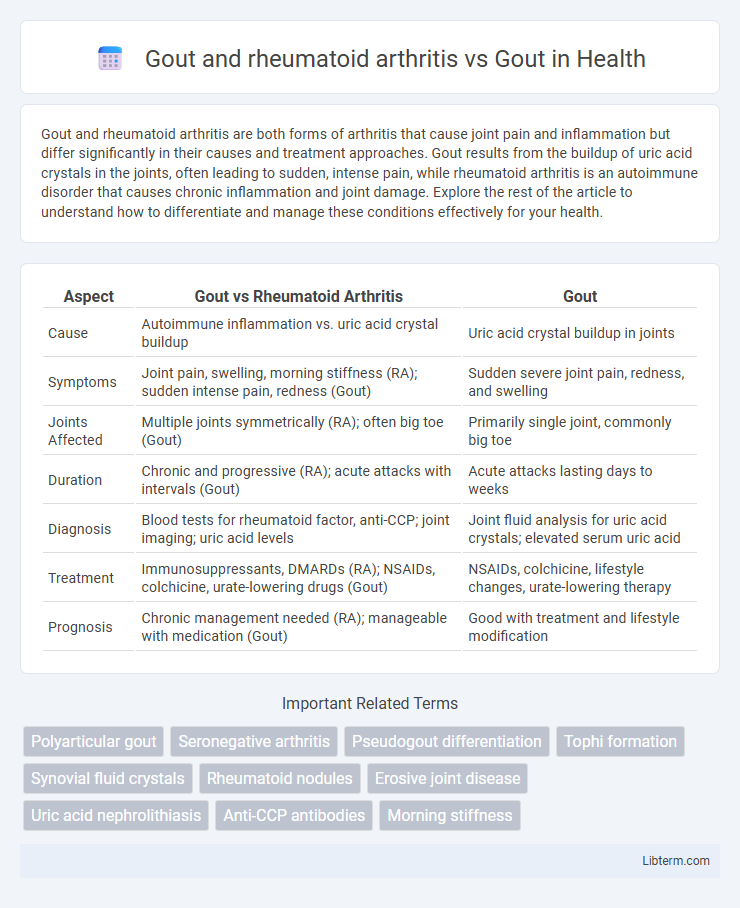
| Aspect | Gout vs Rheumatoid Arthritis | Gout |
|---|---|---|
| Cause | Autoimmune inflammation vs. uric acid crystal buildup | Uric acid crystal buildup in joints |
| Symptoms | Joint pain, swelling, morning stiffness (RA); sudden intense pain, redness (Gout) | Sudden severe joint pain, redness, and swelling |
| Joints Affected | Multiple joints symmetrically (RA); often big toe (Gout) | Primarily single joint, commonly big toe |
| Duration | Chronic and progressive (RA); acute attacks with intervals (Gout) | Acute attacks lasting days to weeks |
| Diagnosis | Blood tests for rheumatoid factor, anti-CCP; joint imaging; uric acid levels | Joint fluid analysis for uric acid crystals; elevated serum uric acid |
| Treatment | Immunosuppressants, DMARDs (RA); NSAIDs, colchicine, urate-lowering drugs (Gout) | NSAIDs, colchicine, lifestyle changes, urate-lowering therapy |
| Prognosis | Chronic management needed (RA); manageable with medication (Gout) | Good with treatment and lifestyle modification |
Understanding Gout: Causes and Symptoms
Gout is a form of inflammatory arthritis caused by the accumulation of uric acid crystals in joints, leading to sudden and severe pain, redness, and swelling, often affecting the big toe. Unlike rheumatoid arthritis, which is an autoimmune disease causing chronic joint inflammation and symmetrical joint damage, gout results from metabolic issues related to hyperuricemia. Early identification of gout symptoms, such as intense joint pain and visible swelling, is crucial for effective management and prevention of recurrent attacks.
Rheumatoid Arthritis: Key Features and Mechanisms
Rheumatoid arthritis (RA) is an autoimmune disorder characterized by chronic inflammation primarily targeting synovial joints, leading to cartilage and bone erosion, contrasting with gout's crystal-induced joint inflammation caused by monosodium urate deposits. RA involves systemic immune dysregulation marked by autoantibodies such as rheumatoid factor (RF) and anti-citrullinated protein antibodies (ACPAs), driving persistent synovitis and joint deformity. Unlike gout, which presents with sudden flare-ups due to urate crystal precipitation, RA manifests as a symmetrical, progressive polyarthritis with complex cytokine-mediated immune responses including tumor necrosis factor-alpha (TNF-a) and interleukin-6 (IL-6).
Gout Versus Rheumatoid Arthritis: Critical Differences
Gout and rheumatoid arthritis (RA) both cause joint inflammation but differ significantly in cause and presentation, with gout caused by uric acid crystal accumulation and RA by autoimmune joint damage. Gout typically presents with sudden, intense pain, redness, and swelling, often affecting the big toe, while RA involves symmetrical joint inflammation with prolonged stiffness and systemic symptoms. Diagnosing gout involves identifying monosodium urate crystals in joint fluid, whereas RA is confirmed through blood tests for rheumatoid factor and anti-CCP antibodies combined with imaging showing joint erosion.
Shared Risk Factors in Gout and Rheumatoid Arthritis
Gout and rheumatoid arthritis share several risk factors including obesity, which increases uric acid production and joint inflammation, and age, as both conditions predominantly affect middle-aged and older adults. Genetic predispositions such as specific HLA gene variants contribute to immune system dysregulation in rheumatoid arthritis and hyperuricemia in gout. Environmental factors like dietary habits rich in purines and alcohol consumption exacerbate inflammation and urate crystal formation common to both diseases.
Diagnostic Challenges: Distinguishing Gout from RA
Gout and rheumatoid arthritis (RA) often present diagnostic challenges due to overlapping symptoms like joint pain and inflammation, complicating differentiation without specific tests. Serum uric acid levels and synovial fluid analysis revealing monosodium urate crystals are pivotal in identifying gout, whereas RA diagnosis relies on detecting rheumatoid factor (RF), anti-citrullinated protein antibodies (ACPA), and characteristic joint imaging findings. Accurate diagnosis ensures targeted treatment, as gout requires urate-lowering therapy while RA management centers on disease-modifying antirheumatic drugs (DMARDs).
Inflammatory Pathways: Gout vs RA
Gout primarily involves the activation of the NLRP3 inflammasome by monosodium urate crystals, leading to the release of interleukin-1b and intense neutrophilic inflammation. Rheumatoid arthritis (RA) is characterized by chronic autoimmune-driven synovial inflammation mediated by autoantibodies, T cells, B cells, and pro-inflammatory cytokines such as tumor necrosis factor-alpha and interleukin-6. Both diseases share inflammatory pathways but differ in triggers and immune cell involvement, with gout showing acute crystal-induced inflammation and RA presenting persistent systemic autoimmunity.
Joint Damage and Disease Progression
Gout causes joint damage primarily through the deposition of monosodium urate crystals, leading to acute inflammation and episodic pain, whereas rheumatoid arthritis (RA) involves chronic autoimmune inflammation targeting synovial joints, resulting in persistent synovitis and progressive joint erosion. Disease progression in gout can be halted or reversed with effective urate-lowering therapy, preventing tophi formation and joint deformities, while RA requires early immunomodulatory treatment to slow irreversible cartilage and bone destruction. Both conditions lead to impaired joint function, but RA typically manifests with symmetrical joint involvement and systemic symptoms, contrasting with the often asymmetric, monoarticular onset of gout.
Treatment Approaches for Gout and Rheumatoid Arthritis
Treatment approaches for gout primarily involve urate-lowering therapies such as allopurinol and febuxostat to reduce serum uric acid levels, along with NSAIDs and colchicine for managing acute attacks. Rheumatoid arthritis treatment focuses on disease-modifying antirheumatic drugs (DMARDs) including methotrexate and biologic agents like TNF inhibitors to control inflammation and prevent joint damage. Both conditions require individualized management plans emphasizing early intervention and lifestyle modifications to optimize outcomes.
Lifestyle Management Strategies
Lifestyle management strategies for gout and rheumatoid arthritis emphasize reducing inflammation and controlling pain through diet, exercise, and stress management. A low-purine diet, adequate hydration, weight management, and limiting alcohol intake are essential for gout to prevent uric acid crystal buildup, while regular low-impact exercise and joint protection techniques improve mobility and reduce joint damage in rheumatoid arthritis. Both conditions benefit from avoiding smoking and adopting anti-inflammatory foods such as omega-3-rich fish and antioxidant-rich fruits and vegetables.
Prognosis and Long-Term Outlook
Gout typically presents with sudden, intense joint pain and swelling, with a generally favorable prognosis when managed through lifestyle modifications and urate-lowering therapy, leading to reduced flare frequency and prevention of joint damage. Rheumatoid arthritis involves persistent systemic inflammation causing progressive joint destruction and deformity, requiring early, aggressive disease-modifying antirheumatic drugs (DMARDs) to improve long-term functional outcomes. Long-term outlook for gout improves significantly with adherence to treatment, while rheumatoid arthritis often necessitates lifelong immunosuppressive therapy to prevent disability and extra-articular complications.
Gout and rheumatoid arthritis Infographic
 libterm.com
libterm.com