Heart block occurs when the electrical signals that control your heartbeat are partially or completely blocked, disrupting normal heart rhythm. This condition can lead to symptoms like dizziness, fatigue, and fainting due to inefficient blood flow. Discover how heart block is diagnosed, treated, and managed by reading the rest of the article.
Table of Comparison
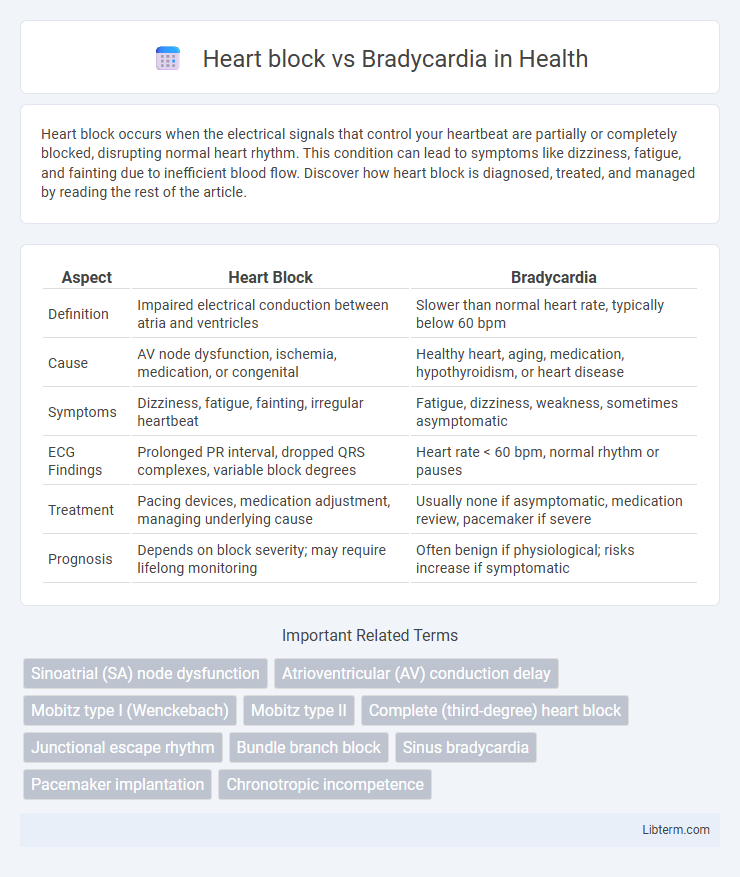
| Aspect | Heart Block | Bradycardia |
|---|---|---|
| Definition | Impaired electrical conduction between atria and ventricles | Slower than normal heart rate, typically below 60 bpm |
| Cause | AV node dysfunction, ischemia, medication, or congenital | Healthy heart, aging, medication, hypothyroidism, or heart disease |
| Symptoms | Dizziness, fatigue, fainting, irregular heartbeat | Fatigue, dizziness, weakness, sometimes asymptomatic |
| ECG Findings | Prolonged PR interval, dropped QRS complexes, variable block degrees | Heart rate < 60 bpm, normal rhythm or pauses |
| Treatment | Pacing devices, medication adjustment, managing underlying cause | Usually none if asymptomatic, medication review, pacemaker if severe |
| Prognosis | Depends on block severity; may require lifelong monitoring | Often benign if physiological; risks increase if symptomatic |
Introduction to Heart Block and Bradycardia
Heart block is a cardiac conduction disorder where the electrical signals between the atria and ventricles are partially or completely impaired, affecting heart rhythm and efficiency. Bradycardia refers to a slower than normal heart rate, typically fewer than 60 beats per minute in adults, which may result from underlying heart block or other cardiac conditions. Both conditions impact cardiac output and require accurate diagnosis to determine appropriate treatment strategies.
Understanding Cardiac Conduction System
Heart block occurs when the electrical signals in the cardiac conduction system are delayed or blocked between the atria and ventricles, disrupting the heart's rhythm and leading to varying degrees of impaired signal transmission. Bradycardia refers to a slower than normal heart rate, often resulting from dysfunction in the sinoatrial (SA) node or conduction pathways, which can manifest independently or alongside heart block. Understanding the cardiac conduction system, including the SA node, atrioventricular (AV) node, bundle of His, and Purkinje fibers, is essential for distinguishing between these conditions and their impact on heart function.
Definition of Heart Block
Heart block is a cardiac conduction disorder characterized by delayed or interrupted electrical signals between the atria and ventricles, impairing normal heart rhythm. It is classified into first-degree, second-degree (Mobitz type I and II), and third-degree (complete) heart block, each varying in severity and clinical implications. Bradycardia, in contrast, refers to a slower than normal heart rate, typically below 60 beats per minute, which may or may not result from heart block.
Definition of Bradycardia
Bradycardia is characterized by a slower than normal heart rate, typically defined as fewer than 60 beats per minute in adults, which can lead to insufficient blood flow to the body. Heart block refers to an impairment in the electrical conduction system of the heart, causing delayed or blocked signals that may result in bradycardia. Unlike heart block, which specifically involves conduction abnormalities, bradycardia can occur due to various causes such as enhanced vagal tone, aging, or medication effects.
Types of Heart Block
Heart block is categorized into three main types: first-degree, second-degree (Type I and Type II), and third-degree, each representing increasing severity of atrioventricular (AV) conduction impairment. First-degree heart block involves prolonged PR interval without missed beats, second-degree Type I (Wenckebach) shows gradual PR lengthening leading to dropped beats, and second-degree Type II features sudden dropped beats without PR prolongation. Third-degree heart block, or complete heart block, occurs when atrial impulses fail to conduct to the ventricles entirely, causing dissociation between atrial and ventricular rhythms, which requires urgent medical intervention.
Causes of Heart Block vs Bradycardia
Heart block primarily results from impaired electrical conduction between the atria and ventricles, often caused by damage from myocardial infarction, fibrosis, or medications like beta-blockers and calcium channel blockers. Bradycardia occurs due to factors such as increased vagal tone, hypothyroidism, electrolyte imbalances, or sinus node dysfunction. Unlike heart block, which involves conduction system abnormalities, bradycardia is characterized by a slowed heart rate originating from sinus node issues or external influences.
Symptoms: Heart Block vs Bradycardia
Heart block symptoms include dizziness, fatigue, palpitations, and episodes of fainting due to disrupted electrical signals in the heart. Bradycardia symptoms often involve slow heart rate, weakness, shortness of breath, and chest pain, reflecting the heart's reduced ability to pump blood efficiently. Both conditions may cause lightheadedness and syncope, but heart block typically shows irregular heartbeats, while bradycardia presents a consistently slow rhythm.
Diagnostic Approaches
Diagnostic approaches for heart block primarily involve electrocardiogram (ECG) analysis to identify the type and degree of conduction delay or interruption within the atrioventricular node or His-Purkinje system. Bradycardia diagnosis includes continuous cardiac monitoring such as Holter monitors or event recorders to assess persistent or intermittent slow heart rates, correlating symptoms like dizziness or fatigue. Advanced imaging or electrophysiological studies may be utilized to differentiate underlying causes and guide treatment strategies for both conditions.
Treatment Differences
Heart block treatment varies based on severity; first-degree block often requires no intervention, while advanced blocks necessitate pacemaker implantation to maintain adequate heart rhythm. Bradycardia treatment depends on underlying causes; reversible factors like medication side effects are addressed by adjusting or discontinuing drugs, and symptomatic bradycardia may require atropine or temporary pacing. Both conditions demand careful evaluation to determine if device therapy or pharmacologic management is appropriate for restoring optimal cardiac function.
Prognosis and Complications
Heart block prognosis varies significantly based on severity and type, with third-degree block posing higher risks such as syncope, heart failure, and sudden cardiac death without pacemaker intervention. Bradycardia generally has a favorable prognosis when due to reversible causes but can lead to fatigue, dizziness, or exacerbation of heart disease if severe and untreated. Complications of untreated heart block include complete heart failure and severe arrhythmias, while chronic bradycardia may precipitate cognitive decline and increased risk of falls in elderly patients.
Heart block Infographic
 libterm.com
libterm.com