Paracentesis is a minimally invasive procedure used to remove excess fluid from the abdominal cavity, often performed to relieve discomfort or diagnose underlying conditions. The technique involves inserting a needle or catheter through the abdominal wall to collect fluid for analysis or therapeutic drainage. Explore the article to understand how paracentesis can benefit your health and when it might be necessary.
Table of Comparison
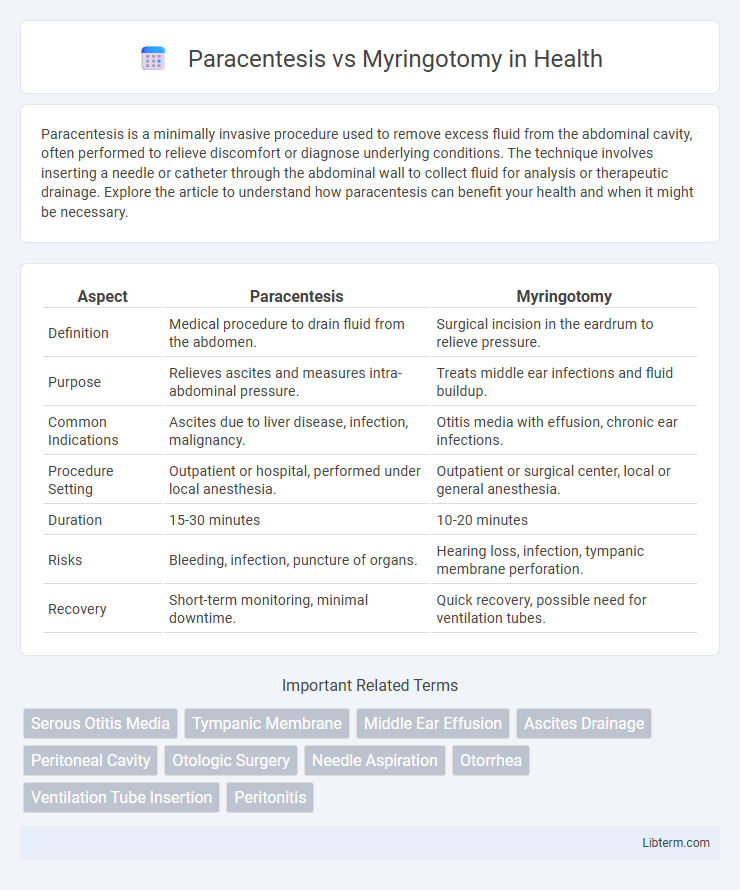
| Aspect | Paracentesis | Myringotomy |
|---|---|---|
| Definition | Medical procedure to drain fluid from the abdomen. | Surgical incision in the eardrum to relieve pressure. |
| Purpose | Relieves ascites and measures intra-abdominal pressure. | Treats middle ear infections and fluid buildup. |
| Common Indications | Ascites due to liver disease, infection, malignancy. | Otitis media with effusion, chronic ear infections. |
| Procedure Setting | Outpatient or hospital, performed under local anesthesia. | Outpatient or surgical center, local or general anesthesia. |
| Duration | 15-30 minutes | 10-20 minutes |
| Risks | Bleeding, infection, puncture of organs. | Hearing loss, infection, tympanic membrane perforation. |
| Recovery | Short-term monitoring, minimal downtime. | Quick recovery, possible need for ventilation tubes. |
Introduction to Paracentesis and Myringotomy
Paracentesis and myringotomy are both minimally invasive procedures used to treat fluid accumulation, but they target different body areas and conditions. Paracentesis involves the insertion of a needle into the peritoneal cavity to remove excess abdominal fluid, commonly performed to diagnose or relieve ascites in liver disease patients. Myringotomy entails creating a small incision in the tympanic membrane to drain middle ear fluid, frequently used to treat chronic otitis media with effusion and prevent recurrent ear infections.
Definitions and Core Differences
Paracentesis is a medical procedure involving the puncture of a body cavity, primarily the abdomen, to remove excess fluid for diagnostic or therapeutic purposes. Myringotomy is a surgical incision made in the tympanic membrane (eardrum) to relieve pressure or drain fluid from the middle ear, often to treat otitis media. The core difference lies in their anatomical focus and purpose: paracentesis targets the abdominal cavity for fluid removal, whereas myringotomy targets the middle ear to alleviate pressure or infection.
Indications for Paracentesis
Paracentesis is primarily indicated for therapeutic relief of symptomatic ascites due to liver cirrhosis, malignancy, or infections like spontaneous bacterial peritonitis, enabling diagnostic analysis of ascitic fluid. This procedure is critical in managing refractory ascites where diuretics fail, and in cases requiring rapid symptomatic improvement from abdominal distension and discomfort. Myringotomy, by contrast, is indicated for relieving middle ear effusions and chronic otitis media, serving a different clinical purpose than paracentesis.
Indications for Myringotomy
Myringotomy is primarily indicated for relieving middle ear effusion in cases of otitis media with persistent fluid causing hearing loss or recurrent infections. It is commonly performed when medical management fails to resolve chronic otitis media or when rapid pressure equalization is needed to alleviate severe ear pain. Paracentesis, in contrast, is a broader term that can refer to puncturing various body cavities, but in otolaryngology, myringotomy specifically targets the tympanic membrane to drain the middle ear.
Procedure Techniques: Paracentesis vs Myringotomy
Paracentesis involves creating a small puncture in the tympanic membrane using a needle or lancet to drain middle ear fluid, typically performed under local anesthesia with minimal tissue disruption. Myringotomy entails making a precise incision in the eardrum using a surgical blade or laser, allowing for fluid drainage and often the insertion of a tympanostomy tube to maintain aeration of the middle ear. Both procedures require sterile techniques and careful visualization of the tympanic membrane to minimize complications and ensure effective fluid removal.
Risks and Complications Compared
Paracentesis carries risks such as bleeding, infection, tympanic membrane perforation, and transient vertigo, while myringotomy complications include persistent perforation, otorrhea, scarring, and rare sensorineural hearing loss. Paracentesis is generally less invasive but has a higher likelihood of discomfort and transient auditory changes. Myringotomy often involves tube placement, increasing the risk of chronic drainage and necessitating potential surgical intervention for persistent complications.
Recovery and Aftercare
Recovery from paracentesis typically involves minimal discomfort and a rapid return to normal activities within a few days, with aftercare focusing on keeping the puncture site clean and monitoring for signs of infection or fluid leakage. Myringotomy recovery generally requires careful protection of the ear from water and avoiding vigorous activities for about a week, as well as monitoring for drainage and possible ear infections due to the small incision or ventilation tube insertion. Both procedures necessitate follow-up evaluations to ensure proper healing and to address any complications promptly.
Efficacy and Outcomes
Paracentesis and myringotomy are both surgical procedures used to alleviate middle ear fluid and pressure, with myringotomy often preferred for its longer-lasting ventilation via tube placement. Studies show myringotomy with tube insertion significantly improves hearing outcomes and reduces recurrence of otitis media compared to simple paracentesis. Paracentesis provides rapid relief but typically requires repeated procedures due to shorter-term efficacy.
Patient Selection Criteria
Paracentesis is primarily selected for patients with acute otitis media presenting with severe ear pain and tympanic membrane bulging, often as a temporary measure to drain middle ear effusion. Myringotomy is favored in recurrent or chronic otitis media cases, especially when accompanied by persistent effusion or hearing loss, and may be combined with tympanostomy tube placement for long-term ventilation. Patient selection hinges on clinical history, frequency of infections, presence of effusion, hearing assessment, and overall impact on quality of life.
Summary: Choosing the Right Procedure
Paracentesis and myringotomy serve distinct purposes, with paracentesis primarily used to remove fluid from the abdominal cavity and myringotomy targeting ear infections by draining fluid from the middle ear. The choice between these procedures depends on the specific medical condition: paracentesis is indicated for ascites management or diagnostic fluid sampling, while myringotomy is ideal for treating persistent otitis media with effusion. Accurate diagnosis and evaluation of symptoms guide clinicians to select the appropriate intervention, optimizing patient outcomes and minimizing complications.
Paracentesis Infographic
 libterm.com
libterm.com