Body Dysmorphic Disorder causes individuals to obsess over perceived flaws in their appearance, often leading to significant emotional distress and impaired daily functioning. Treatment options include cognitive-behavioral therapy and medication, which can help manage symptoms and improve quality of life. Discover how recognizing the signs and seeking professional support can transform your understanding of this condition in the full article.
Table of Comparison
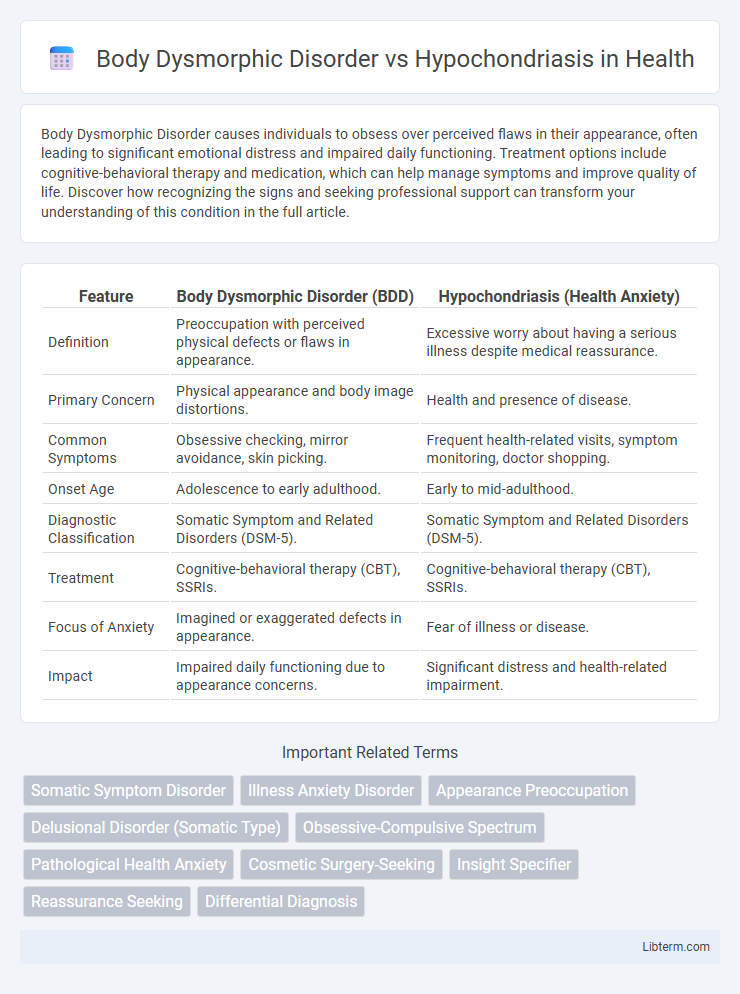
| Feature | Body Dysmorphic Disorder (BDD) | Hypochondriasis (Health Anxiety) |
|---|---|---|
| Definition | Preoccupation with perceived physical defects or flaws in appearance. | Excessive worry about having a serious illness despite medical reassurance. |
| Primary Concern | Physical appearance and body image distortions. | Health and presence of disease. |
| Common Symptoms | Obsessive checking, mirror avoidance, skin picking. | Frequent health-related visits, symptom monitoring, doctor shopping. |
| Onset Age | Adolescence to early adulthood. | Early to mid-adulthood. |
| Diagnostic Classification | Somatic Symptom and Related Disorders (DSM-5). | Somatic Symptom and Related Disorders (DSM-5). |
| Treatment | Cognitive-behavioral therapy (CBT), SSRIs. | Cognitive-behavioral therapy (CBT), SSRIs. |
| Focus of Anxiety | Imagined or exaggerated defects in appearance. | Fear of illness or disease. |
| Impact | Impaired daily functioning due to appearance concerns. | Significant distress and health-related impairment. |
Understanding Body Dysmorphic Disorder (BDD)
Body Dysmorphic Disorder (BDD) is a mental health condition characterized by an obsessive focus on perceived flaws in physical appearance, which are often unnoticeable to others. Unlike Hypochondriasis, where individuals fear having serious illnesses, BDD centers on distress about body image and leads to repetitive behaviors such as mirror checking or excessive grooming. Effective treatment for BDD includes cognitive-behavioral therapy (CBT) and selective serotonin reuptake inhibitors (SSRIs) to reduce obsessive thoughts and improve daily functioning.
What is Hypochondriasis?
Hypochondriasis, also known as illness anxiety disorder, is a mental health condition characterized by an excessive preoccupation with having a serious illness despite medical evaluations showing no significant health problems. Individuals with hypochondriasis frequently misinterpret normal bodily sensations or minor symptoms as indicative of severe diseases, leading to persistent anxiety and frequent doctor visits. This disorder differs from body dysmorphic disorder, which centers on obsessive concerns with perceived physical flaws rather than fears of illness.
Key Differences Between BDD and Hypochondriasis
Body Dysmorphic Disorder (BDD) centers on an intense, irrational focus on perceived physical flaws, often leading to compulsive behaviors to hide or fix the defect. Hypochondriasis, or illness anxiety disorder, is characterized by excessive worry about having or developing serious medical conditions despite minimal or no symptoms. Key differences include BDD's preoccupation with appearance versus hypochondriasis's concern with health, with BDD involving body image disturbances and hypochondriasis involving health anxiety and frequent medical consultations.
Overlapping Symptoms and Misconceptions
Body Dysmorphic Disorder (BDD) and Hypochondriasis share overlapping symptoms such as excessive preoccupation with perceived flaws--BDD centers on physical appearance flaws while Hypochondriasis focuses on fears of having serious illnesses. Both disorders drive repetitive behaviors like mirror checking, medical consultations, and reassurance-seeking, often leading to significant distress and interference in daily functioning. Misconceptions include mistaking BDD for mere vanity or Hypochondriasis for simple health anxiety, underscoring the need for accurate diagnosis and targeted treatment strategies.
Causes and Risk Factors
Body Dysmorphic Disorder (BDD) primarily stems from a combination of genetic predisposition, neurobiological abnormalities, and environmental influences such as childhood trauma or cultural pressure emphasizing physical appearance. Hypochondriasis, also known as illness anxiety disorder, often arises from a history of serious illness, heightened sensitivity to bodily sensations, and dysfunctional cognitive patterns related to health anxiety. Both disorders share risk factors like anxiety disorders and stressful life events but diverge significantly in their focus: BDD centers on perceived physical defects, while hypochondriasis concerns fears of having a serious medical condition.
Psychological and Social Impacts
Body Dysmorphic Disorder (BDD) primarily leads to severe psychological distress driven by obsessive preoccupation with perceived physical flaws, resulting in social withdrawal, anxiety, and impaired daily functioning. Hypochondriasis, characterized by excessive health anxiety and fear of serious illness, causes persistent psychological distress and significant social impairment due to frequent medical consultations and avoidance of perceived health risks. Both disorders profoundly disrupt social relationships and reduce quality of life, with BDD emphasizing appearance-related distress and hypochondriasis centering on health-related fears.
Diagnosis: BDD vs Hypochondriasis
Diagnosis of Body Dysmorphic Disorder (BDD) centers on the presence of preoccupation with perceived physical flaws that are minor or nonexistent, causing significant distress or impairment. Hypochondriasis, now classified as Illness Anxiety Disorder, involves excessive worry about having a serious illness despite minimal or no medical evidence. Differentiating BDD from Hypochondriasis relies on assessing whether the individual's focus is predominantly on appearance-related concerns versus health-related fears.
Treatment Options for Both Disorders
Cognitive-behavioral therapy (CBT) is a primary treatment option for Body Dysmorphic Disorder (BDD), aimed at reducing obsessive thoughts and compulsive behaviors related to perceived physical flaws. Selective serotonin reuptake inhibitors (SSRIs) are also commonly prescribed to alleviate symptoms for both BDD and Hypochondriasis, targeting underlying anxiety and depression. Exposure and response prevention (ERP) techniques are effective in Hypochondriasis treatment by gradually desensitizing patients to health-related fears and reducing avoidance behaviors.
Coping Strategies and Support Systems
Effective coping strategies for Body Dysmorphic Disorder (BDD) emphasize cognitive-behavioral therapy (CBT) to address distorted self-image, while hypochondriasis benefits from exposure therapy and reassurance techniques to reduce health anxiety. Support systems involving family education and peer support groups enhance treatment adherence and emotional resilience for individuals with both disorders. Integration of professional mental health services alongside community support fosters sustained recovery and symptom management.
When to Seek Professional Help
Seek professional help for Body Dysmorphic Disorder (BDD) when obsessive concerns about perceived physical flaws cause significant distress or impair daily functioning. In cases of Hypochondriasis, consult a healthcare provider if excessive worry about having a serious illness leads to frequent doctor visits or anxiety despite negative medical evaluations. Early intervention by mental health specialists can prevent worsening symptoms and improve coping strategies for both disorders.
Body Dysmorphic Disorder Infographic
 libterm.com
libterm.com