Thrombosis occurs when a blood clot forms inside a blood vessel, obstructing the flow of blood through the circulatory system. This condition can lead to severe health complications, including stroke or heart attack, depending on the location of the clot. Discover the causes, symptoms, and treatments of thrombosis to protect your health in the following article.
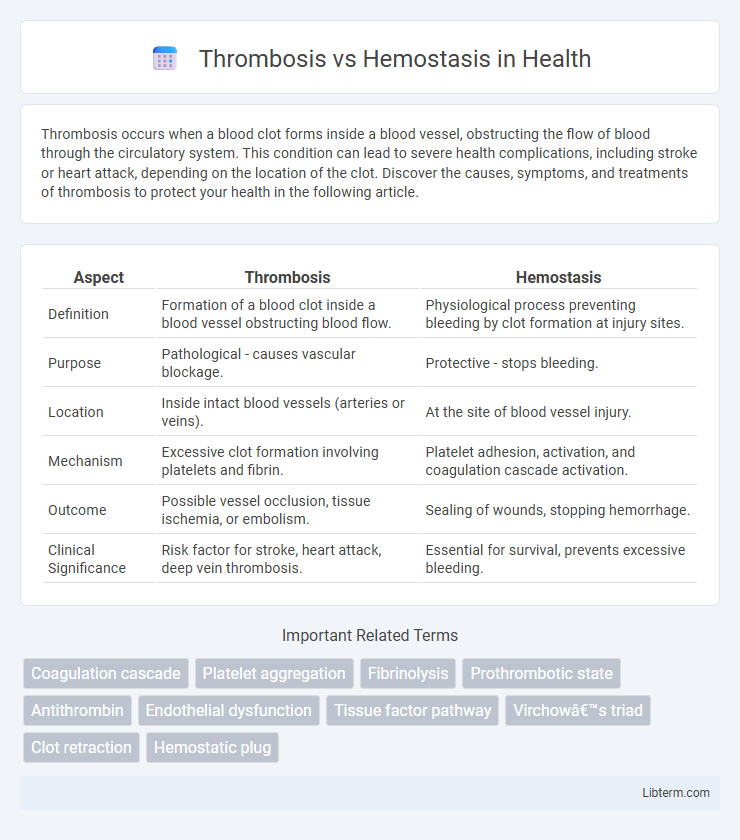
Table of Comparison
| Aspect | Thrombosis | Hemostasis |
|---|---|---|
| Definition | Formation of a blood clot inside a blood vessel obstructing blood flow. | Physiological process preventing bleeding by clot formation at injury sites. |
| Purpose | Pathological - causes vascular blockage. | Protective - stops bleeding. |
| Location | Inside intact blood vessels (arteries or veins). | At the site of blood vessel injury. |
| Mechanism | Excessive clot formation involving platelets and fibrin. | Platelet adhesion, activation, and coagulation cascade activation. |
| Outcome | Possible vessel occlusion, tissue ischemia, or embolism. | Sealing of wounds, stopping hemorrhage. |
| Clinical Significance | Risk factor for stroke, heart attack, deep vein thrombosis. | Essential for survival, prevents excessive bleeding. |
Introduction to Thrombosis and Hemostasis
Thrombosis is the pathological formation of blood clots within blood vessels, obstructing normal blood flow and potentially leading to conditions such as stroke or myocardial infarction. Hemostasis is the physiological process that stops bleeding by forming a stable blood clot at the site of vascular injury, involving vascular constriction, platelet activation, and coagulation cascade. Understanding the balance between thrombosis and hemostasis is critical for preventing excessive bleeding and thrombotic diseases.
Definition of Thrombosis
Thrombosis is the pathological formation of a blood clot within a blood vessel, obstructing normal blood flow and potentially leading to tissue damage or organ dysfunction. It differs from hemostasis, which is the physiological process that stops bleeding by forming a balanced clot at the site of vascular injury. Understanding the mechanisms of thrombosis is crucial for diagnosing and treating thrombotic disorders such as deep vein thrombosis and stroke.
Definition of Hemostasis
Hemostasis is the physiological process that stops bleeding at the site of an injured blood vessel by forming a stable blood clot through vasoconstriction, platelet aggregation, and coagulation. Thrombosis occurs when this clotting process becomes excessive or inappropriate, leading to the formation of clots within intact blood vessels that can obstruct blood flow. Understanding hemostasis is crucial in differentiating normal clotting from pathological thrombus formation.
Key Mechanisms: Thrombosis vs Hemostasis
Thrombosis involves the pathological formation of blood clots within blood vessels, driven by endothelial injury, platelet activation, and the coagulation cascade leading to fibrin mesh formation. Hemostasis is a tightly regulated physiological process that prevents bleeding by balancing vasoconstriction, platelet plug formation, and controlled activation of the coagulation system to stabilize the clot without excessive thrombosis. Key mechanisms in thrombosis include persistent endothelial dysfunction and hypercoagulability, whereas hemostasis requires precise interaction among platelets, coagulation factors, and fibrinolytic pathways to maintain vascular integrity.
Risk Factors and Triggers
Thrombosis risk factors include inherited clotting disorders, prolonged immobility, obesity, smoking, cancer, and surgery, which promote abnormal clot formation within blood vessels. Hemostasis involves triggers such as vascular injury, platelet activation, and the coagulation cascade to prevent bleeding by forming a localized clot at the injury site. Disruption or imbalance in these processes can increase susceptibility to pathological thrombosis or bleeding disorders.
Clinical Manifestations
Thrombosis manifests clinically through symptoms such as swelling, pain, warmth, and redness in the affected limb due to venous obstruction or localized ischemia in arterial involvement. Hemostasis disorders can present as excessive bleeding, spontaneous bruising, mucosal hemorrhages, or prolonged bleeding times stemming from platelet dysfunction or coagulation factor deficiencies. Differentiating these conditions is critical for diagnosis and treatment, with thrombosis often leading to complications like pulmonary embolism and hemostasis disorders predisposing patients to hemorrhagic events.
Diagnostic Differences
Thrombosis diagnosis primarily relies on imaging techniques such as Doppler ultrasound, CT angiography, or MRI to detect abnormal blood clots within vessels, supported by blood tests measuring D-dimer levels and coagulation profiles. Hemostasis evaluation centers on laboratory assays like prothrombin time (PT), activated partial thromboplastin time (aPTT), platelet function tests, and bleeding time to assess the blood's ability to clot properly. Differentiating thrombosis from hemostasis disorders involves integrating clinical presentation with targeted diagnostic tests to identify clot formation versus bleeding tendencies.
Management and Treatment Approaches
Management of thrombosis primarily involves anticoagulant therapies such as heparin, warfarin, or direct oral anticoagulants (DOACs) to inhibit clot formation and prevent embolism. Hemostasis treatment focuses on controlling bleeding by using agents like vitamin K, platelet transfusions, or antifibrinolytic drugs to restore clotting function. In critical cases, mechanical interventions such as thrombectomy for thrombosis or surgical hemostasis may be necessary to manage complications effectively.
Complications and Prognosis
Thrombosis, the formation of abnormal blood clots within vessels, often leads to complications such as stroke, myocardial infarction, and pulmonary embolism, significantly increasing morbidity and mortality rates. Hemostasis, the physiological process that stops bleeding, can be disrupted either by excessive clotting or insufficient clot formation, resulting in complications like hemorrhage or thrombosis. Prognosis varies; untreated thrombosis carries high risks of severe complications and death, while effective management of hemostasis disorders improves patient outcomes and reduces relapse.
Prevention Strategies
Prevention strategies for thrombosis emphasize anticoagulant medications such as heparin and warfarin to inhibit clot formation, alongside lifestyle changes like regular exercise, smoking cessation, and maintaining healthy weight. Hemostasis prevention focuses on managing bleeding risks by monitoring platelet function and coagulation factors, especially in patients with clotting disorders or those undergoing surgery. Both conditions require tailored approaches based on individual risk factors, ensuring optimal balance between clot prevention and bleeding control.
Thrombosis Infographic
 libterm.com
libterm.com