Iatrogenic conditions arise as unintended consequences of medical treatment or diagnostic procedures, often complicating patient health and recovery. Understanding the causes and prevention strategies of iatrogenic harm is crucial for improving healthcare outcomes and minimizing risks. Discover how to recognize and manage iatrogenic issues effectively by reading the full article.
Table of Comparison
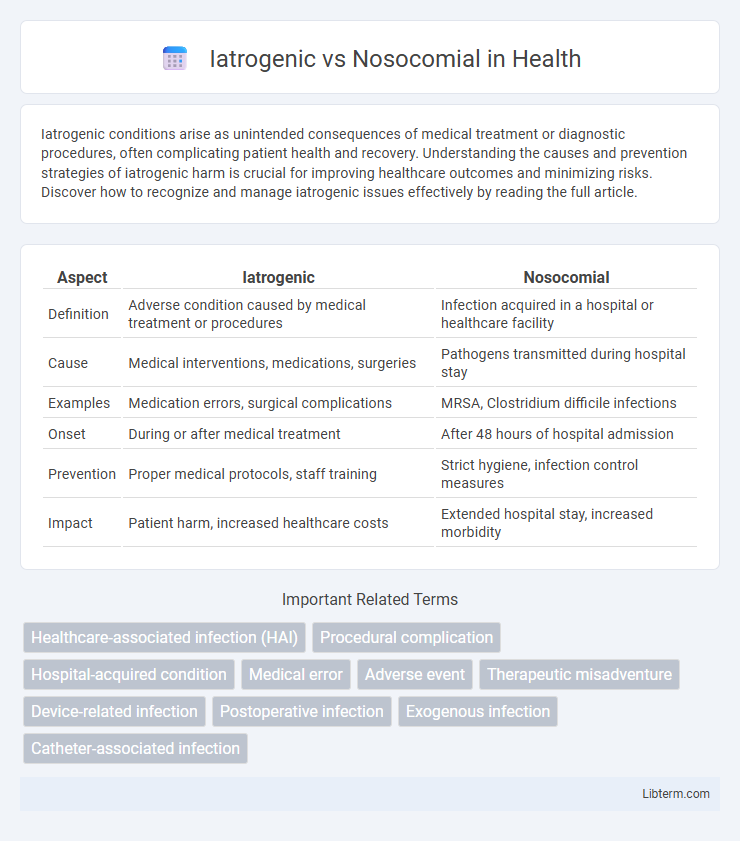
| Aspect | Iatrogenic | Nosocomial |
|---|---|---|
| Definition | Adverse condition caused by medical treatment or procedures | Infection acquired in a hospital or healthcare facility |
| Cause | Medical interventions, medications, surgeries | Pathogens transmitted during hospital stay |
| Examples | Medication errors, surgical complications | MRSA, Clostridium difficile infections |
| Onset | During or after medical treatment | After 48 hours of hospital admission |
| Prevention | Proper medical protocols, staff training | Strict hygiene, infection control measures |
| Impact | Patient harm, increased healthcare costs | Extended hospital stay, increased morbidity |
Understanding Iatrogenic and Nosocomial: Key Definitions
Iatrogenic conditions arise directly from medical interventions, including treatments, procedures, or diagnostic tests, often as unintended side effects or complications. Nosocomial infections, also known as hospital-acquired infections, develop during a hospital stay and are not present or incubating at the time of admission, commonly caused by pathogens like Staphylococcus aureus or Clostridium difficile. Differentiating between iatrogenic and nosocomial factors is essential for improving patient safety, minimizing risk, and enhancing clinical outcomes.
Historical Overview of Iatrogenic and Nosocomial Events
Iatrogenic events have been recognized since ancient medical practices, with Hippocrates warning about the potential harm of treatments dating back to 400 BCE, while nosocomial infections gained prominence with the 19th-century work of Ignaz Semmelweis, who identified hand hygiene as crucial in reducing hospital-acquired infections. The historical evolution of iatrogenic harm includes advancements in surgery and pharmacology, revealing both therapeutic benefits and unintended consequences. Nosocomial infection control improved significantly after the discovery of germ theory and implementation of antiseptic techniques in hospitals.
Major Causes of Iatrogenic Conditions
Iatrogenic conditions primarily arise from medical interventions such as surgery, medication errors, and diagnostic procedures, which can inadvertently cause complications or adverse effects in patients. Common major causes include adverse drug reactions, surgical errors, anesthesia complications, and hospital-acquired infections linked to invasive treatments. Understanding these factors is essential for improving patient safety and reducing iatrogenic harm within healthcare settings.
Common Sources of Nosocomial Infections
Nosocomial infections, also known as hospital-acquired infections, commonly originate from contaminated medical devices, surgical procedures, and healthcare personnel's hands. Common sources include urinary catheters, ventilators, intravenous lines, and improperly sterilized surgical instruments, which facilitate the transmission of pathogens like Staphylococcus aureus and Pseudomonas aeruginosa. These infections are distinct from iatrogenic infections, which specifically result from direct medical treatment or intervention errors.
Diagnostic Differences: Iatrogenic vs Nosocomial
Iatrogenic conditions arise directly from medical interventions or treatments, often identified through patient history linking symptoms to recent procedures, medications, or diagnostic tests. Nosocomial infections, by contrast, are hospital-acquired infections diagnosed based on the onset of symptoms at least 48 hours after admission, with laboratory cultures confirming hospital-specific pathogens. Differentiating these requires analyzing timing, clinical context, and microbiological data to determine whether adverse effects stem from therapeutic actions or opportunistic infections within the healthcare setting.
Clinical Implications and Patient Outcomes
Iatrogenic conditions arise directly from medical interventions, often leading to complications such as medication errors or surgical injuries that can worsen patient prognosis and extend hospital stays. Nosocomial infections, acquired during hospitalization, significantly increase morbidity and mortality rates due to pathogens like MRSA and Clostridium difficile, complicating recovery and escalating healthcare costs. Understanding the distinction between these factors is crucial for implementing targeted strategies to minimize adverse events, improve clinical outcomes, and enhance overall patient safety.
Prevention Strategies in Healthcare Settings
Iatrogenic infections, caused by medical interventions, and nosocomial infections, acquired in healthcare environments, require targeted prevention strategies such as strict adherence to sterilization protocols and proper hand hygiene among healthcare workers. Implementing antimicrobial stewardship programs reduces the risk of antibiotic resistance associated with both types of infections. Regular staff training and patient monitoring protocols further minimize infection rates and enhance patient safety in clinical settings.
Risk Factors Contributing to Iatrogenic and Nosocomial Cases
Iatrogenic cases arise primarily from medical interventions such as surgeries, catheter insertions, or medication errors, with risk factors including poor procedural technique, inadequate sterilization, and improper drug administration. Nosocomial infections mainly result from prolonged hospital stays, invasive devices like ventilators or central lines, and compromised patient immunity, often exacerbated by lapses in infection control protocols. Both types of cases share risk contributors like inadequate hand hygiene, environmental contamination, and failure to adhere to clinical guidelines, increasing patient vulnerability to adverse outcomes.
Legal and Ethical Considerations
Iatrogenic injuries, caused by medical treatment or diagnostic procedures, often raise legal issues related to medical malpractice and informed consent violations, requiring thorough documentation and patient communication. Nosocomial infections, acquired in healthcare settings, present ethical challenges in infection control and patient safety, demanding strict adherence to protocols to prevent harm and potential liability. Both require healthcare providers to balance duty of care with transparent disclosure to uphold ethical standards and minimize legal repercussions.
Future Directions in Reducing Healthcare-Associated Harms
Emerging technologies such as artificial intelligence and machine learning are being developed to predict and prevent iatrogenic and nosocomial complications by analyzing patient data in real-time. Enhanced infection control protocols, including antimicrobial stewardship and rapid diagnostic testing, show promise in reducing nosocomial infections in healthcare settings. Future efforts emphasize personalized medicine and advanced training for healthcare professionals to minimize treatment-related harms and optimize patient safety outcomes.
Iatrogenic Infographic
 libterm.com
libterm.com