Pathogenicity refers to the ability of an organism, such as bacteria, viruses, or fungi, to cause disease in a host. Understanding the mechanisms behind pathogenicity, including how pathogens invade, evade immune responses, and produce toxins, is crucial for developing effective treatments. Discover more about how pathogenicity impacts health and disease progression in the rest of this article.
Table of Comparison
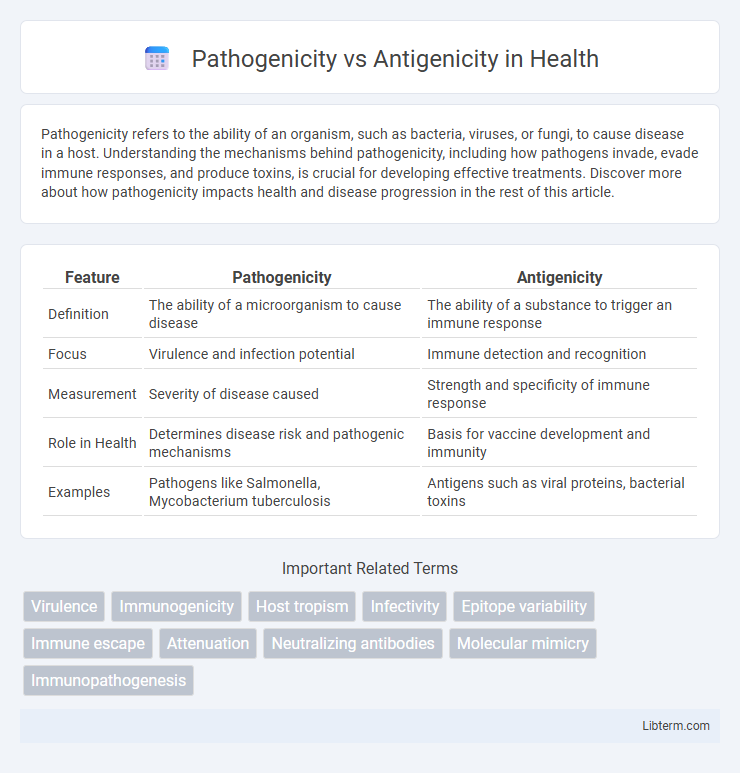
| Feature | Pathogenicity | Antigenicity |
|---|---|---|
| Definition | The ability of a microorganism to cause disease | The ability of a substance to trigger an immune response |
| Focus | Virulence and infection potential | Immune detection and recognition |
| Measurement | Severity of disease caused | Strength and specificity of immune response |
| Role in Health | Determines disease risk and pathogenic mechanisms | Basis for vaccine development and immunity |
| Examples | Pathogens like Salmonella, Mycobacterium tuberculosis | Antigens such as viral proteins, bacterial toxins |
Introduction to Pathogenicity and Antigenicity
Pathogenicity refers to the ability of a microorganism to cause disease in a host, determined by its virulence factors such as toxins, enzymes, and invasion mechanisms. Antigenicity is the capacity of a pathogen or substance to induce an immune response by being recognized as an antigen by the host's immune system. Understanding the distinction between pathogenicity and antigenicity is crucial for developing vaccines and therapeutic interventions targeting infectious diseases.
Defining Pathogenicity: Mechanisms of Disease
Pathogenicity refers to the ability of a microorganism to cause disease by invading host tissues, evading immune responses, and producing toxins or enzymes that damage cells. Mechanisms of disease include adhesion to host cells, colonization, immune suppression, and the release of exotoxins or endotoxins that disrupt normal physiological functions. Understanding these factors is crucial for developing treatments targeting the microbial factors responsible for infection and disease progression.
Understanding Antigenicity: Immune System Recognition
Antigenicity refers to a molecule's ability to be recognized by the immune system, specifically by antibodies or T-cell receptors, triggering an immune response. Understanding antigenicity is crucial for vaccine development as it determines how effectively an antigen can stimulate immune defenses against pathogens. Unlike pathogenicity, which relates to a pathogen's ability to cause disease, antigenicity centers on immune system recognition and response efficacy.
Key Differences Between Pathogenicity and Antigenicity
Pathogenicity refers to the ability of a microorganism to cause disease in a host, while antigenicity is the capacity of a substance to provoke an immune response by being recognized as an antigen. Key differences include that pathogenicity involves factors like virulence, invasion, and toxin production, whereas antigenicity centers on the molecular structures, such as proteins or polysaccharides, that trigger antibody formation. Pathogenicity directly impacts disease severity, whereas antigenicity influences immune detection and the development of immunity or vaccines.
Molecular Determinants of Pathogenicity
Molecular determinants of pathogenicity include specific virulence factors such as toxins, enzymes, and adhesion molecules that enable pathogens to invade host tissues and evade the immune response. Genetic elements like pathogenicity islands and plasmids encode these factors, influencing a microbe's ability to cause disease. Antigenicity, distinct from pathogenicity, is determined by surface molecules like proteins and polysaccharides that trigger host immune recognition without necessarily contributing to virulence.
Factors Influencing Antigenicity
Antigenicity is influenced by factors such as molecular size, chemical complexity, and structural stability of the antigen, which determine its ability to induce an immune response. Pathogenicity refers to the capacity of an organism to cause disease, while antigenicity relates to the recognition of the antigen by the host's immune system. Variations in antigenic determinants, dosage of antigen exposure, and genetic makeup of the host also significantly impact antigenicity.
Pathogenicity and Antigenicity in Viral Infections
Pathogenicity in viral infections refers to the ability of a virus to cause disease by damaging host tissues, disrupting normal cellular functions, and evading the immune system. Antigenicity describes the capacity of viral components, such as surface proteins or capsid antigens, to be recognized by the host immune system, triggering an immune response. Variations in antigenicity influence the effectiveness of immune recognition and vaccine design, while pathogenicity determines the severity and clinical outcomes of the viral infection.
Impact on Vaccine Development
Pathogenicity determines the severity of disease caused by a microorganism, while antigenicity defines its ability to trigger an immune response, both critically influencing vaccine design. High antigenicity with low pathogenicity is ideal for vaccines, ensuring effective immune activation without causing illness. Identifying antigenic determinants and minimizing pathogenic effects accelerate the development of safe and effective vaccines against infectious diseases.
Clinical Implications: Diagnosis and Treatment
Pathogenicity determines the severity and progression of infectious diseases, influencing clinical diagnosis by highlighting the need for early identification of virulent strains to prevent complications. Antigenicity guides diagnostic tests such as serological assays by detecting specific immune responses, enabling precise identification of pathogens. Understanding both factors informs treatment strategies, including the choice of targeted antimicrobial therapy and vaccine development to enhance immune protection.
Future Perspectives in Pathogenicity and Antigenicity Research
Future research in pathogenicity aims to decode microbial mechanisms at the molecular level to develop targeted therapies and precision vaccines. Advances in antigenicity studies focus on enhancing immunogenic profiles through bioinformatics and synthetic biology to improve vaccine efficacy against emerging variants. Integrating multi-omics data promises to revolutionize disease prevention by predicting pathogen evolution and host immune responses.
Pathogenicity Infographic
 libterm.com
libterm.com