Neutrophilic monocytic cells play a crucial role in the immune system by responding to infections and inflammation through phagocytosis and cytokine production. These cells are essential for your body's defense mechanism, helping to identify and eliminate harmful pathogens. Discover more about how neutrophilic monocytic cells function and their importance by reading the rest of the article.
Table of Comparison
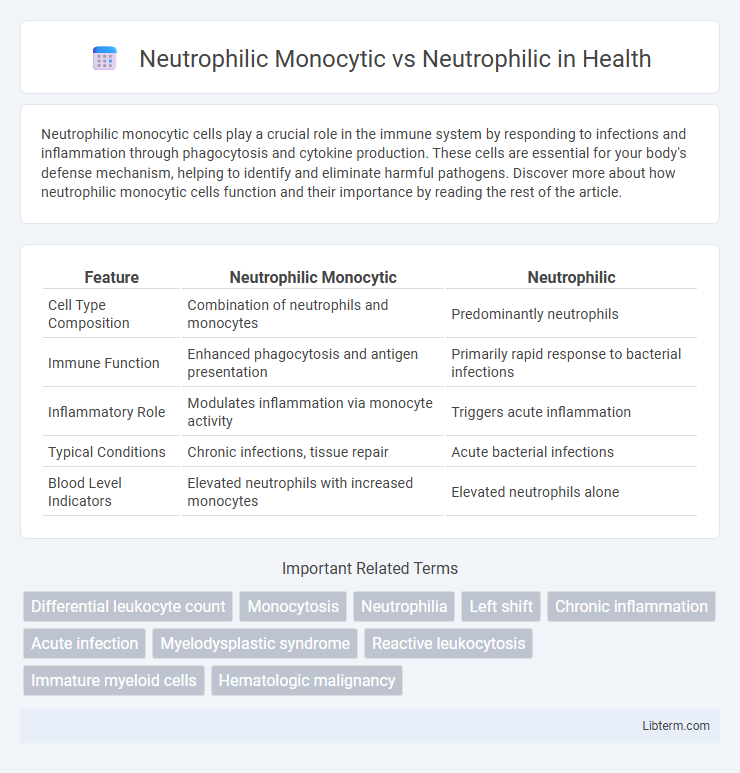
| Feature | Neutrophilic Monocytic | Neutrophilic |
|---|---|---|
| Cell Type Composition | Combination of neutrophils and monocytes | Predominantly neutrophils |
| Immune Function | Enhanced phagocytosis and antigen presentation | Primarily rapid response to bacterial infections |
| Inflammatory Role | Modulates inflammation via monocyte activity | Triggers acute inflammation |
| Typical Conditions | Chronic infections, tissue repair | Acute bacterial infections |
| Blood Level Indicators | Elevated neutrophils with increased monocytes | Elevated neutrophils alone |
Introduction to Neutrophilic and Neutrophilic Monocytic Responses
Neutrophilic responses primarily involve the rapid activation and recruitment of neutrophils, the most abundant type of white blood cells, to sites of infection or injury, where they execute phagocytosis and release antimicrobial agents. Neutrophilic monocytic responses integrate the actions of both neutrophils and monocytes, a subset of leukocytes that differentiate into macrophages and dendritic cells, enhancing pathogen clearance and inflammation regulation. The interplay between neutrophils and monocytes in these responses is crucial for orchestrating innate immunity and shaping the adaptive immune response.
Defining Neutrophilic Inflammation
Neutrophilic inflammation is characterized by the predominance of neutrophils, a type of white blood cell essential for the body's immediate defense against bacterial infections and tissue injury. Neutrophilic monocytic inflammation involves both neutrophils and monocytes, where monocytes contribute to prolonged immune responses and tissue repair mechanisms. Differentiating between these inflammatory patterns is crucial for accurate diagnosis and targeted treatment of various acute and chronic inflammatory diseases.
Understanding Neutrophilic Monocytic Infiltration
Neutrophilic monocytic infiltration involves the simultaneous presence of neutrophils and monocytes within tissue, indicating a mixed inflammatory response often seen in chronic infections or autoimmune conditions. In contrast, neutrophilic infiltration predominantly features neutrophils alone, typically signaling acute inflammation or bacterial infections. Understanding the cellular composition and behavior of neutrophilic monocytic infiltration enhances the diagnosis and treatment of inflammatory diseases by identifying the underlying immune mechanisms.
Cellular Composition: Neutrophils vs Monocytes
Neutrophilic monocytic cellular composition involves a mixed population dominated by neutrophils and monocytes, whereas neutrophilic composition is primarily composed of neutrophils alone. Neutrophils are key phagocytic cells responsible for rapid response to infection, while monocytes have a dual role in phagocytosis and differentiation into macrophages or dendritic cells. The relative abundance of monocytes in neutrophilic monocytic compositions reflects an enhanced inflammatory and immune-regulatory function compared to solely neutrophilic profiles.
Pathophysiology of Neutrophilic and Neutrophilic Monocytic Conditions
Neutrophilic conditions involve an elevated presence of neutrophils, key immune cells responsible for rapid response and phagocytosis during acute inflammation and infection, driven by cytokines like G-CSF. Neutrophilic monocytic conditions feature simultaneous increases in neutrophils and monocytes, reflecting both acute and chronic inflammatory responses with monocytes differentiating into macrophages and dendritic cells, contributing to sustained immune activation. The pathophysiology of these conditions centers on dysregulated hematopoiesis and immune signaling pathways, including overproduction of pro-inflammatory cytokines such as IL-1, IL-6, and TNF-a, leading to tissue damage and altered immune homeostasis.
Key Differences in Immune Function
Neutrophilic-monocytic cells combine properties of neutrophils and monocytes, playing a dual role in phagocytosis and antigen presentation, whereas neutrophilic cells primarily engage in rapid pathogen engulfment and release of antimicrobial substances. Neutrophilic-monocytic cells contribute more extensively to bridging innate and adaptive immunity through cytokine secretion and activation of T-cells. Neutrophils act as first responders during acute infection, specializing in microbial killing and inflammation without the long-term immune memory functions attributed to monocytes.
Clinical Manifestations and Disease Associations
Neutrophilic monocytic infiltration often presents with combined symptoms of inflammation and immune dysregulation, commonly seen in infections like bacterial sepsis and autoimmune diseases such as rheumatoid arthritis. In contrast, neutrophilic infiltration alone is predominantly associated with acute bacterial infections and acute inflammatory responses, characterized by rapid onset of fever, localized pain, and swelling. Disease associations of neutrophilic monocytic patterns include chronic inflammatory disorders and certain hematologic malignancies, whereas neutrophilic patterns primarily correlate with acute, localized tissue injury and pyogenic infections.
Diagnostic Approaches for Differentiating Both Conditions
Diagnostic approaches for differentiating Neutrophilic Monocytic leukemia from Neutrophilic leukemoid reactions primarily rely on comprehensive hematologic evaluations, including peripheral blood smear analysis and immunophenotyping by flow cytometry to identify distinct cell surface markers. Molecular genetic testing, such as PCR and cytogenetic analysis, detects specific mutations or chromosomal abnormalities characteristic of Neutrophilic Monocytic leukemia, aiding in differentiation from reactive neutrophilia. Bone marrow biopsy with histopathological assessment provides critical insights into cellular morphology and marrow infiltration patterns, further distinguishing malignant proliferations from benign neutrophilic responses.
Treatment Strategies and Therapeutic Outcomes
Neutrophilic monocytic inflammation requires treatment strategies that target both neutrophil and monocyte activation pathways, often involving corticosteroids combined with immunomodulatory agents for better therapeutic outcomes. Neutrophilic inflammation typically responds to therapies focused on neutrophil suppression, such as corticosteroids or targeted biologics like anti-IL-8 antibodies, resulting in reduced tissue damage and inflammation. Tailoring treatments based on the cellular profile enhances efficacy, reducing relapse rates and improving long-term disease control in inflammatory conditions.
Prognosis and Clinical Implications
Neutrophilic monocytic leukemia often presents with a more aggressive clinical course and poorer prognosis compared to neutrophilic leukemia due to the involvement of both neutrophil and monocyte lineages, leading to more complex immune dysregulation. Prognostic factors in neutrophilic monocytic cases include higher white blood cell counts and increased blast cells, which correlate with resistance to standard therapies and higher relapse rates. Clinical management requires tailored approaches combining intensive chemotherapy and targeted treatments to address the distinct pathophysiology and improve patient outcomes.
Neutrophilic Monocytic Infographic
 libterm.com
libterm.com