Lichen planus is a chronic inflammatory condition affecting the skin, mucous membranes, nails, and hair, characterized by purple, itchy, flat-topped bumps. Its exact cause is unknown, but it is believed to be linked to an immune system response triggered by factors such as stress, infections, or certain medications. Discover more about the symptoms, causes, and treatment options to manage your condition effectively in the rest of this article.
Table of Comparison
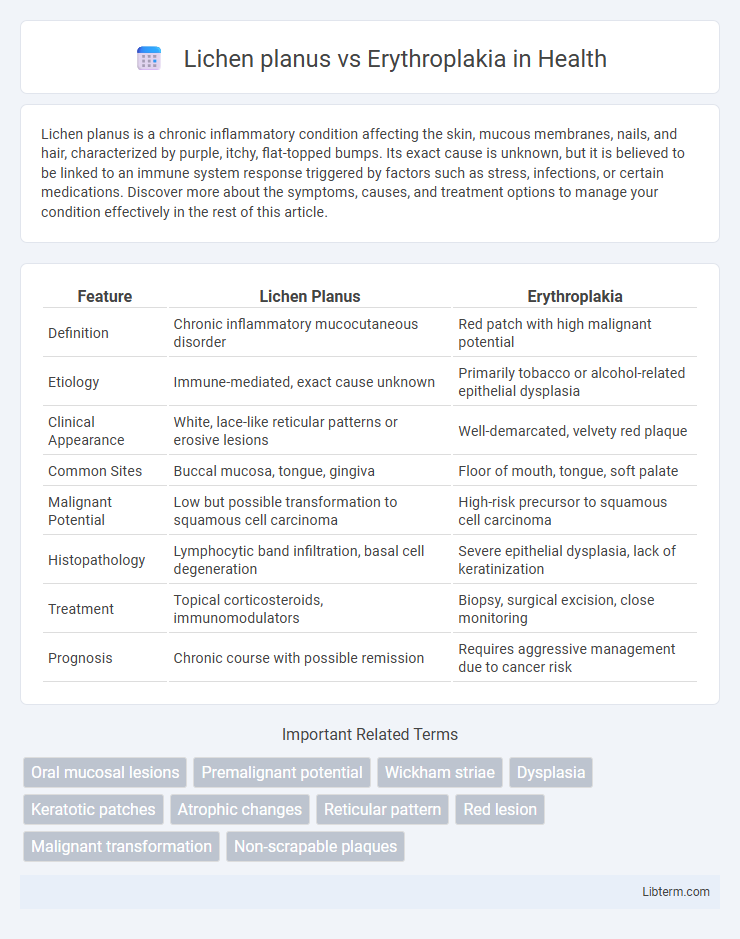
| Feature | Lichen Planus | Erythroplakia |
|---|---|---|
| Definition | Chronic inflammatory mucocutaneous disorder | Red patch with high malignant potential |
| Etiology | Immune-mediated, exact cause unknown | Primarily tobacco or alcohol-related epithelial dysplasia |
| Clinical Appearance | White, lace-like reticular patterns or erosive lesions | Well-demarcated, velvety red plaque |
| Common Sites | Buccal mucosa, tongue, gingiva | Floor of mouth, tongue, soft palate |
| Malignant Potential | Low but possible transformation to squamous cell carcinoma | High-risk precursor to squamous cell carcinoma |
| Histopathology | Lymphocytic band infiltration, basal cell degeneration | Severe epithelial dysplasia, lack of keratinization |
| Treatment | Topical corticosteroids, immunomodulators | Biopsy, surgical excision, close monitoring |
| Prognosis | Chronic course with possible remission | Requires aggressive management due to cancer risk |
Overview of Lichen Planus and Erythroplakia
Lichen planus is a chronic inflammatory condition characterized by purplish, polygonal, pruritic papules primarily affecting the skin and oral mucosa, often with a reticular white pattern known as Wickham's striae. Erythroplakia presents as a red, velvety patch on mucous membranes, with a high risk of malignant transformation, particularly in the oral cavity. Both conditions require clinical evaluation and biopsy due to their potential for premalignant changes, with lichen planus linked to autoimmune mechanisms and erythroplakia commonly associated with tobacco and alcohol use.
Etiology and Risk Factors
Lichen planus is a chronic inflammatory condition linked to immune-mediated mechanisms, with potential triggers including stress, hepatitis C infection, and certain medications. Erythroplakia, primarily a precancerous lesion, arises from chronic irritation factors such as tobacco use, alcohol consumption, and human papillomavirus (HPV) infection. Both conditions exhibit distinct etiologies, with lichen planus involving autoimmune responses and erythroplakia associated predominantly with carcinogenic risk factors.
Epidemiology and Demographics
Lichen planus predominantly affects middle-aged adults, with a higher prevalence in females, especially those aged 30-60 years, while erythroplakia is more common in older adults, mainly males over 50 years with a history of tobacco or alcohol use. The global prevalence of oral lichen planus ranges from 0.5% to 2%, contrasting with erythroplakia, a rarer lesion with a prevalence below 0.02% but a higher potential for malignant transformation. Geographic variation exists, with lichen planus more frequently reported in European and Asian populations, whereas erythroplakia incidence correlates with regions of high tobacco consumption, such as South Asia.
Clinical Features and Presentation
Lichen planus presents with violaceous, flat-topped papules often accompanied by Wickham striae and commonly affects the buccal mucosa, wrists, and ankles, causing pruritus and discomfort. Erythroplakia manifests as a well-demarcated, erythematous plaque most frequently on the floor of the mouth, ventral tongue, or soft palate, with a high risk of malignant transformation. Clinical examination reveals the chronic, reticular pattern of lichen planus contrasting with the smooth, velvety, and often asymptomatic erythroplakia lesions.
Histopathological Differences
Lichen planus exhibits a band-like lymphocytic infiltrate at the dermoepidermal junction, with hypergranulosis and saw-tooth-shaped rete ridges, whereas erythroplakia shows marked epithelial dysplasia with loss of normal maturation and often full-thickness atypia. Civatte bodies are characteristic of lichen planus, representing apoptotic keratinocytes, while erythroplakia frequently demonstrates increased mitotic figures and nuclear pleomorphism indicative of premalignant changes. The basement membrane remains intact in lichen planus, contrasting with the disrupted architecture and potential invasion seen in erythroplakia histopathology.
Diagnosis: Criteria and Tools
Diagnosis of lichen planus involves clinical examination and confirmation by biopsy, highlighting characteristic saw-tooth lymphocytic infiltrates and basal cell degeneration. Erythroplakia diagnosis relies on identifying persistent, well-demarcated red patches with a high risk of dysplasia or carcinoma, usually confirmed through biopsy and histopathological analysis. Both conditions benefit from adjunctive tools such as direct immunofluorescence for lichen planus and toluidine blue staining or autofluorescence for erythroplakia to improve detection accuracy.
Malignant Transformation Potential
Lichen planus carries a low but notable risk of malignant transformation, estimated at approximately 1-3%, predominantly progressing to oral squamous cell carcinoma. Erythroplakia demonstrates a significantly higher malignant transformation potential, with reported rates up to 20-50%, often associated with severe dysplasia or carcinoma in situ at diagnosis. Early recognition and biopsy of erythroplakia are critical due to its aggressive premalignant nature compared to the relatively indolent course of lichen planus.
Management and Treatment Options
Lichen planus treatment primarily involves corticosteroids, such as topical clobetasol or systemic prednisone for severe cases, alongside immunomodulatory agents like tacrolimus to reduce inflammatory response. Erythroplakia management requires prompt biopsy due to its high malignant transformation risk, with treatment often involving surgical excision or laser therapy to remove dysplastic tissue. Regular follow-up and monitoring for recurrence or malignant progression are critical for both conditions to ensure early intervention and optimal patient outcomes.
Prognosis and Follow-Up Strategies
Lichen planus typically presents a chronic course with a low risk of malignant transformation, necessitating regular clinical follow-up every 6 to 12 months to monitor for potential changes or symptom progression. Erythroplakia carries a significantly higher risk of progressing to squamous cell carcinoma, requiring more aggressive surveillance including biopsy confirmation and frequent follow-up visits every 3 months to detect early dysplastic or malignant changes. Early diagnosis and consistent monitoring are crucial in both conditions to improve patient prognosis and prevent malignant progression.
Prevention and Patient Education
Effective prevention of Lichen planus involves avoiding triggers such as stress, certain medications, and allergens, while maintaining good oral hygiene helps reduce exacerbations. Educating patients about erythroplakia emphasizes early detection and the importance of eliminating risk factors like tobacco and alcohol use to prevent malignant transformation. Regular dental check-ups and self-examination empower patients to monitor for suspicious mucosal changes in both conditions, facilitating timely intervention.
Lichen planus Infographic
 libterm.com
libterm.com