Insulin resistance occurs when cells in your muscles, fat, and liver don't respond well to insulin, making it harder to absorb glucose from the bloodstream. This condition often leads to higher blood sugar levels and can increase the risk of type 2 diabetes and other metabolic disorders. Discover more about the causes, symptoms, and management strategies in the rest of this article.
Table of Comparison
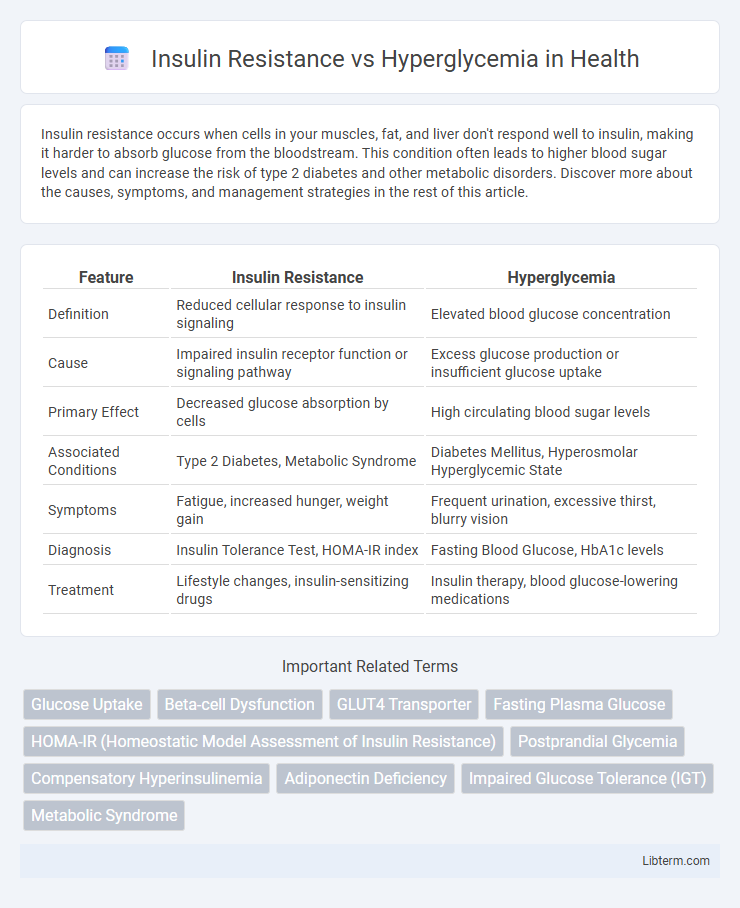
| Feature | Insulin Resistance | Hyperglycemia |
|---|---|---|
| Definition | Reduced cellular response to insulin signaling | Elevated blood glucose concentration |
| Cause | Impaired insulin receptor function or signaling pathway | Excess glucose production or insufficient glucose uptake |
| Primary Effect | Decreased glucose absorption by cells | High circulating blood sugar levels |
| Associated Conditions | Type 2 Diabetes, Metabolic Syndrome | Diabetes Mellitus, Hyperosmolar Hyperglycemic State |
| Symptoms | Fatigue, increased hunger, weight gain | Frequent urination, excessive thirst, blurry vision |
| Diagnosis | Insulin Tolerance Test, HOMA-IR index | Fasting Blood Glucose, HbA1c levels |
| Treatment | Lifestyle changes, insulin-sensitizing drugs | Insulin therapy, blood glucose-lowering medications |
Understanding Insulin Resistance
Insulin resistance occurs when cells in muscles, fat, and the liver respond poorly to insulin, impairing glucose uptake and leading to elevated blood sugar levels. This diminished sensitivity forces the pancreas to produce more insulin, often resulting in hyperinsulinemia before hyperglycemia manifests. Understanding insulin resistance is critical for preventing Type 2 diabetes, as it represents an early metabolic dysfunction that precedes chronic high blood glucose.
What is Hyperglycemia?
Hyperglycemia is a medical condition characterized by elevated blood glucose levels exceeding the normal range, typically above 130 mg/dL fasting or 180 mg/dL postprandial. It occurs when the body either produces insufficient insulin or cells become resistant to insulin's effects, impairing glucose uptake. Persistent hyperglycemia is a hallmark of diabetes mellitus and can lead to severe complications such as neuropathy, retinopathy, and cardiovascular disease if not properly managed.
Causes of Insulin Resistance
Insulin resistance primarily arises from genetic factors, obesity, and sedentary lifestyle, which impair the body's ability to utilize insulin effectively. Chronic inflammation, excess fatty acids, and hormonal imbalances also contribute to the reduced insulin sensitivity of muscle, fat, and liver cells. Unlike hyperglycemia, which is an elevated blood glucose level often resulting from insulin resistance, the root cause of insulin resistance lies in cellular dysfunction and metabolic disturbances that block insulin signaling pathways.
Causes of Hyperglycemia
Hyperglycemia primarily results from insulin resistance, where muscle, fat, and liver cells fail to respond effectively to insulin, leading to elevated blood glucose levels. Pancreatic beta-cell dysfunction also contributes by reducing insulin secretion, exacerbating hyperglycemia. Other causes include stress-induced hormonal changes, excessive carbohydrate intake, and certain medications that impair glucose metabolism.
Key Differences: Insulin Resistance vs Hyperglycemia
Insulin resistance occurs when cells in muscles, fat, and the liver do not respond well to insulin and cannot easily absorb glucose from the bloodstream, leading to increased insulin production by the pancreas. Hyperglycemia refers to elevated blood glucose levels resulting from insufficient insulin action or secretion, often seen in diabetes mellitus. While insulin resistance is a cellular-level dysfunction affecting insulin signaling pathways, hyperglycemia is a measurable condition of high blood sugar, frequently caused by or exacerbating insulin resistance.
Signs and Symptoms to Watch For
Insulin resistance often presents with signs such as increased hunger, fatigue, and darkened skin patches called acanthosis nigricans, whereas hyperglycemia typically manifests through excessive thirst, frequent urination, and blurred vision. Monitoring these symptoms is crucial, as insulin resistance can progress to type 2 diabetes, characterized by chronic hyperglycemia. Early detection through these markers allows for timely intervention to prevent complications like neuropathy and cardiovascular disease.
Health Risks Associated with Each Condition
Insulin resistance increases the risk of developing type 2 diabetes, cardiovascular disease, and metabolic syndrome due to impaired glucose uptake by cells. Hyperglycemia, characterized by elevated blood glucose levels, can lead to complications such as diabetic neuropathy, retinopathy, kidney damage, and increased risk of cardiovascular events. Both conditions contribute significantly to chronic health issues, emphasizing the importance of early detection and management to prevent long-term organ damage.
Diagnosis: How Doctors Differentiate
Doctors differentiate insulin resistance from hyperglycemia primarily through diagnostic tests such as fasting blood glucose, oral glucose tolerance test (OGTT), and hemoglobin A1c levels. Insulin resistance is often identified by elevated fasting insulin levels alongside normal or slightly elevated blood glucose, while hyperglycemia is confirmed by persistently high blood glucose readings above 126 mg/dL fasting or 200 mg/dL post-OGTT. Advanced diagnostic tools like the HOMA-IR index are used to quantify insulin resistance more precisely, aiding in distinguishing these conditions for appropriate treatment planning.
Prevention and Management Strategies
Effective prevention and management of insulin resistance and hyperglycemia center on maintaining balanced blood sugar levels through diet, exercise, and weight control. Implementing a low-glycemic index diet rich in fiber and engaging in regular physical activity enhances insulin sensitivity and reduces glucose spikes. Monitoring blood glucose levels and using medications such as metformin when prescribed further help manage these conditions and prevent progression to type 2 diabetes.
When to Seek Medical Help
Seek medical help for insulin resistance if you experience persistent fatigue, increased thirst, frequent urination, or unexplained weight changes, as these signs indicate potential prediabetes or type 2 diabetes. Hyperglycemia symptoms such as blurred vision, headache, abdominal pain, and rapid heartbeat require immediate evaluation to prevent diabetic ketoacidosis or other complications. Early diagnosis through blood glucose testing and timely intervention can significantly reduce the risk of long-term cardiovascular and neurological damage.
Insulin Resistance Infographic
 libterm.com
libterm.com