Hypernatremia occurs when there is an elevated sodium level in the blood, often caused by dehydration or excessive salt intake. This imbalance can lead to symptoms such as confusion, muscle weakness, and seizures if left untreated. Discover more about the causes, symptoms, and treatments of hypernatremia in the rest of this article.
Table of Comparison
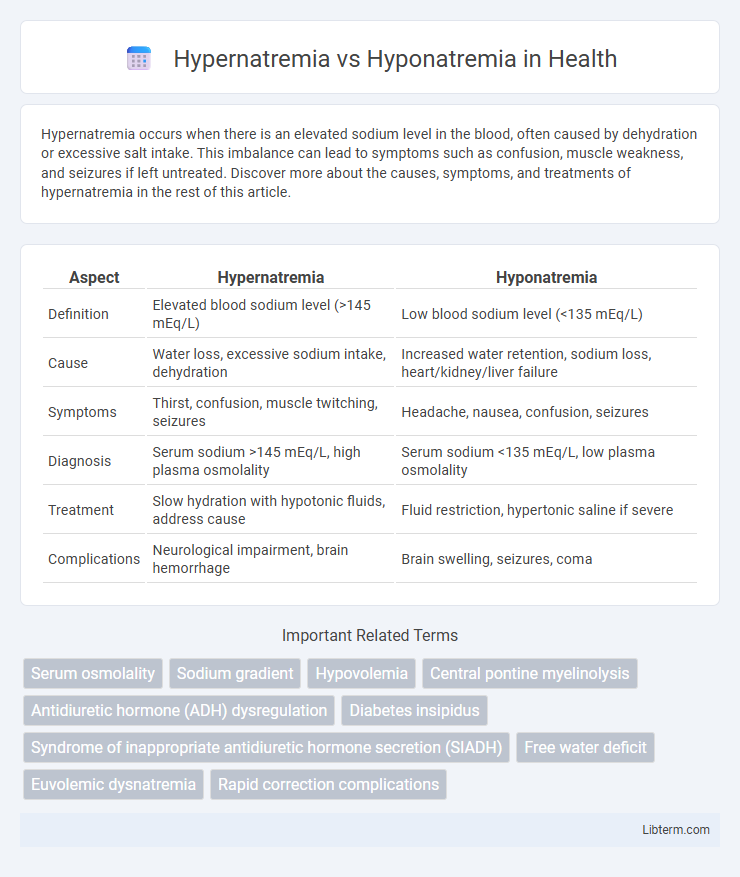
| Aspect | Hypernatremia | Hyponatremia |
|---|---|---|
| Definition | Elevated blood sodium level (>145 mEq/L) | Low blood sodium level (<135 mEq/L) |
| Cause | Water loss, excessive sodium intake, dehydration | Increased water retention, sodium loss, heart/kidney/liver failure |
| Symptoms | Thirst, confusion, muscle twitching, seizures | Headache, nausea, confusion, seizures |
| Diagnosis | Serum sodium >145 mEq/L, high plasma osmolality | Serum sodium <135 mEq/L, low plasma osmolality |
| Treatment | Slow hydration with hypotonic fluids, address cause | Fluid restriction, hypertonic saline if severe |
| Complications | Neurological impairment, brain hemorrhage | Brain swelling, seizures, coma |
Introduction to Hypernatremia and Hyponatremia
Hypernatremia is characterized by an elevated serum sodium concentration exceeding 145 mEq/L, often resulting from water deficit or excessive sodium intake, leading to cellular dehydration and neurological symptoms. Hyponatremia, defined by serum sodium levels below 135 mEq/L, typically arises from water retention or sodium loss, causing cellular swelling and neurological dysfunction. Both electrolyte imbalances reflect critical disturbances in fluid balance and require accurate diagnosis for appropriate management.
Definitions and Key Differences
Hypernatremia is defined by a serum sodium concentration exceeding 145 mEq/L, indicating hyperosmolarity due to water deficit relative to sodium, whereas hyponatremia involves serum sodium levels below 135 mEq/L, reflecting a relative excess of water compared to sodium. The key differences lie in pathophysiology: hypernatremia results from water loss or sodium gain, causing cellular dehydration, while hyponatremia stems from excess water retention or sodium loss, leading to cellular swelling. Clinical manifestations vary accordingly, with hypernatremia causing neurologic symptoms such as irritability and seizures, and hyponatremia presenting with headache, nausea, and potential cerebral edema.
Causes of Hypernatremia
Hypernatremia primarily results from water loss exceeding sodium loss, often due to dehydration, diabetes insipidus, or excessive salt intake. Conditions such as impaired thirst mechanisms, severe diarrhea, or use of diuretics can also precipitate hypernatremia. Unlike hyponatremia, which involves low serum sodium levels typically caused by fluid overload or sodium loss, hypernatremia reflects an elevated sodium concentration due to relative water deficit.
Causes of Hyponatremia
Hyponatremia is primarily caused by excessive water retention due to conditions such as heart failure, liver cirrhosis, and syndrome of inappropriate antidiuretic hormone secretion (SIADH). Other causes include chronic kidney disease, adrenal insufficiency, and the use of certain diuretics or medications that impair sodium balance. Understanding these underlying factors is crucial for accurate diagnosis and effective management of hyponatremia.
Clinical Manifestations
Hypernatremia presents with clinical manifestations such as confusion, lethargy, muscle twitching, and seizures due to hyperosmolarity causing cellular dehydration, particularly in the brain. In contrast, hyponatremia manifests with headache, nausea, vomiting, confusion, and in severe cases, seizures and coma, stemming from cellular swelling and cerebral edema. Both conditions require prompt recognition of neurological symptoms to prevent irreversible brain damage.
Diagnostic Criteria and Laboratory Findings
Hypernatremia is diagnosed when serum sodium levels exceed 145 mEq/L, often accompanied by hyperosmolality and increased serum chloride, reflecting water deficit or sodium excess. Hyponatremia is identified by serum sodium levels below 135 mEq/L, with corresponding hypoosmolality and variable urine sodium that helps differentiate between euvolemic, hypervolemic, or hypovolemic states. Laboratory findings in hypernatremia typically show elevated blood urea nitrogen and creatinine indicating dehydration, whereas hyponatremia lab results may reveal low serum uric acid and variable urine osmolality depending on the underlying cause.
Risk Factors and Predisposing Conditions
Hypernatremia risk factors include dehydration, diabetes insipidus, and excessive sodium intake, often seen in elderly or critically ill patients with impaired thirst mechanisms. Hyponatremia is commonly associated with conditions like heart failure, liver cirrhosis, renal insufficiency, and syndrome of inappropriate antidiuretic hormone secretion (SIADH). Both electrolyte imbalances can be precipitated by medications such as diuretics and can occur in hospitalized patients with altered fluid balance.
Complications and Prognosis
Hypernatremia often leads to neurological complications such as seizures, confusion, and coma due to cellular dehydration, while hyponatremia can cause cerebral edema, resulting in headaches, nausea, and in severe cases, brain herniation. Prognosis for hypernatremia depends on the rapidity of sodium correction; overly rapid correction risks cerebral hemorrhage, whereas untreated hyponatremia increases risk of permanent neurological damage and mortality in severe cases. Both electrolyte imbalances require careful management to prevent long-term cognitive impairment and life-threatening complications.
Treatment Strategies and Management
Treatment strategies for hypernatremia primarily involve gradual correction of serum sodium levels through controlled administration of hypotonic fluids, such as 5% dextrose in water or half-normal saline, to prevent cerebral edema. Hyponatremia management depends on severity and etiology, with options including fluid restriction for euvolemic or hypervolemic hyponatremia, hypertonic saline infusion for symptomatic or severe cases, and addressing underlying causes like SIADH or heart failure. Close monitoring of serum sodium and neurological status is critical in both conditions to avoid rapid shifts that can lead to osmotic demyelination syndrome or cerebral edema.
Prevention and Patient Education
Prevention of hypernatremia centers on maintaining adequate hydration and monitoring sodium intake, especially in elderly or at-risk patients, while preventing hyponatremia involves avoiding excessive water intake and managing underlying conditions like heart failure or SIADH. Patient education should emphasize recognizing early symptoms such as confusion or muscle cramps and the importance of regular medical follow-up to adjust fluid and electrolyte balance. Clear guidance on dietary sodium and fluid restrictions tailored to individual health conditions optimizes outcomes and reduces the risk of severe electrolyte imbalances.
Hypernatremia Infographic
 libterm.com
libterm.com