Hepatitis is an inflammation of the liver caused by viral infections, toxins, or autoimmune diseases, significantly impacting liver function and overall health. Timely diagnosis and effective treatment are crucial to prevent serious complications like liver cirrhosis or cancer. Explore the rest of this article to understand the types, symptoms, and management strategies of hepatitis for your well-being.
Table of Comparison
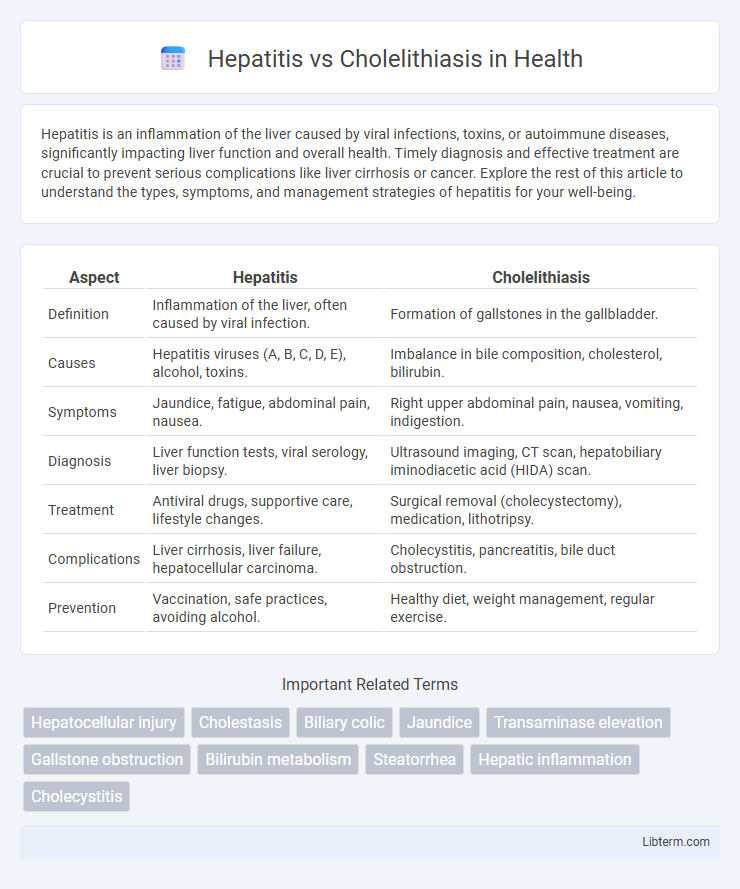
| Aspect | Hepatitis | Cholelithiasis |
|---|---|---|
| Definition | Inflammation of the liver, often caused by viral infection. | Formation of gallstones in the gallbladder. |
| Causes | Hepatitis viruses (A, B, C, D, E), alcohol, toxins. | Imbalance in bile composition, cholesterol, bilirubin. |
| Symptoms | Jaundice, fatigue, abdominal pain, nausea. | Right upper abdominal pain, nausea, vomiting, indigestion. |
| Diagnosis | Liver function tests, viral serology, liver biopsy. | Ultrasound imaging, CT scan, hepatobiliary iminodiacetic acid (HIDA) scan. |
| Treatment | Antiviral drugs, supportive care, lifestyle changes. | Surgical removal (cholecystectomy), medication, lithotripsy. |
| Complications | Liver cirrhosis, liver failure, hepatocellular carcinoma. | Cholecystitis, pancreatitis, bile duct obstruction. |
| Prevention | Vaccination, safe practices, avoiding alcohol. | Healthy diet, weight management, regular exercise. |
Understanding Hepatitis and Cholelithiasis
Hepatitis is an inflammatory liver condition caused by viral infections, toxins, or autoimmune diseases, leading to symptoms such as jaundice, fatigue, and liver dysfunction. Cholelithiasis refers to the formation of gallstones within the gallbladder, often resulting in biliary colic, nausea, and potential complications like cholecystitis. Understanding the pathophysiology, diagnostic imaging, and laboratory markers like elevated liver enzymes for hepatitis and ultrasonography identifying gallstones is crucial for accurate differentiation and effective treatment.
Causes and Risk Factors
Hepatitis is primarily caused by viral infections such as hepatitis A, B, C, D, and E, with risk factors including intravenous drug use, unprotected sex, and exposure to contaminated blood. Cholelithiasis, or gallstone formation, is linked to cholesterol supersaturation in bile, with risk factors including obesity, female gender, advanced age, and rapid weight loss. Both conditions involve distinct pathophysiological mechanisms influenced by genetic predispositions and lifestyle factors.
Symptoms Comparison
Hepatitis typically presents with symptoms such as jaundice, fatigue, abdominal pain, dark urine, and nausea, reflecting liver inflammation and impaired liver function. In contrast, cholelithiasis commonly causes episodes of intense right upper quadrant pain, often after fatty meals, along with nausea and vomiting due to gallstone obstruction of the bile ducts. Unlike hepatitis, cholelithiasis rarely results in systemic symptoms like fever or jaundice unless complicated by cholecystitis or choledocholithiasis.
Pathophysiology Differences
Hepatitis is characterized by inflammation and necrosis of hepatocytes primarily due to viral infections, autoimmune responses, or toxins, impairing liver function and bile production. In contrast, cholelithiasis involves the formation of gallstones within the gallbladder caused by imbalances in bile components such as cholesterol, bilirubin, and bile salts, leading to obstruction and inflammation. The pathophysiology of hepatitis centers on hepatocellular injury and immune-mediated liver damage, whereas cholelithiasis results from gallbladder dysmotility and supersaturation of bile promoting crystal nucleation.
Diagnostic Approaches
Hepatitis diagnosis primarily relies on serological tests detecting viral antigens or antibodies, liver function tests indicating elevated ALT and AST, and imaging studies like ultrasound to assess liver inflammation. Cholelithiasis diagnosis centers on abdominal ultrasound, which identifies gallstones and gallbladder wall thickness, supplemented by hepatobiliary iminodiacetic acid (HIDA) scans or magnetic resonance cholangiopancreatography (MRCP) for bile duct evaluation. Both conditions require differential diagnosis using laboratory markers and imaging to distinguish liver parenchymal injury from biliary obstruction.
Treatment Modalities
Hepatitis treatment modalities vary based on the type, with antiviral medications like interferon and direct-acting antivirals (DAAs) used for viral hepatitis, while supportive care including hydration and liver function monitoring is essential for acute cases. Cholelithiasis treatment focuses on symptom relief and stone removal, with laparoscopic cholecystectomy as the standard surgical intervention, and oral bile acid therapy or extracorporeal shock wave lithotripsy being options for non-surgical candidates. Both conditions require tailored approaches that address the underlying pathology and patient-specific factors to optimize clinical outcomes.
Complications and Prognosis
Hepatitis can lead to severe complications including liver cirrhosis, hepatic encephalopathy, and hepatocellular carcinoma, significantly impacting prognosis with potential for chronic liver failure if untreated. Cholelithiasis raises the risk of gallbladder inflammation, biliary obstruction, and pancreatitis, which may require surgical intervention to prevent chronic complications. Prognosis in hepatitis depends on viral etiology and treatment response, while cholelithiasis prognosis improves with timely gallstone removal and management of biliary complications.
Prevention Strategies
Preventing hepatitis primarily involves vaccination, practicing safe sex, avoiding sharing needles, and ensuring safe blood transfusions to reduce viral transmission risks. Cholelithiasis prevention focuses on maintaining a healthy weight through regular exercise, a balanced diet low in saturated fats and cholesterol, and avoiding rapid weight loss that can promote gallstone formation. Both conditions benefit from routine medical check-ups to identify risk factors early and implement tailored lifestyle modifications.
Lifestyle Modifications
Adopting lifestyle modifications plays a crucial role in managing both hepatitis and cholelithiasis by reducing symptom severity and preventing disease progression. For hepatitis, maintaining a balanced diet rich in antioxidants and avoiding alcohol supports liver function and reduces inflammation. In cholelithiasis, a low-fat diet combined with regular physical activity helps prevent gallstone formation and promotes bile flow efficiency.
Frequently Asked Questions
Hepatitis is an inflammation of the liver often caused by viral infections such as Hepatitis A, B, or C, whereas cholelithiasis refers to the formation of gallstones in the gallbladder, which can block bile flow and cause pain. Common questions about hepatitis include symptoms like jaundice, fatigue, and liver enzyme levels, while cholelithiasis FAQs focus on causes such as cholesterol imbalance, gallbladder inflammation, and treatment options like cholecystectomy. Both conditions require medical evaluation through blood tests, imaging studies, and sometimes biopsy to guide appropriate management and prevent complications.
Hepatitis Infographic
 libterm.com
libterm.com