Syncope refers to a temporary loss of consciousness caused by a sudden drop in blood flow to the brain, often resulting in fainting. Identifying the underlying causes, such as cardiac issues or dehydration, is critical for effective treatment and prevention of future episodes. Discover how understanding the types, symptoms, and management of syncope can help safeguard your health throughout the rest of this article.
Table of Comparison
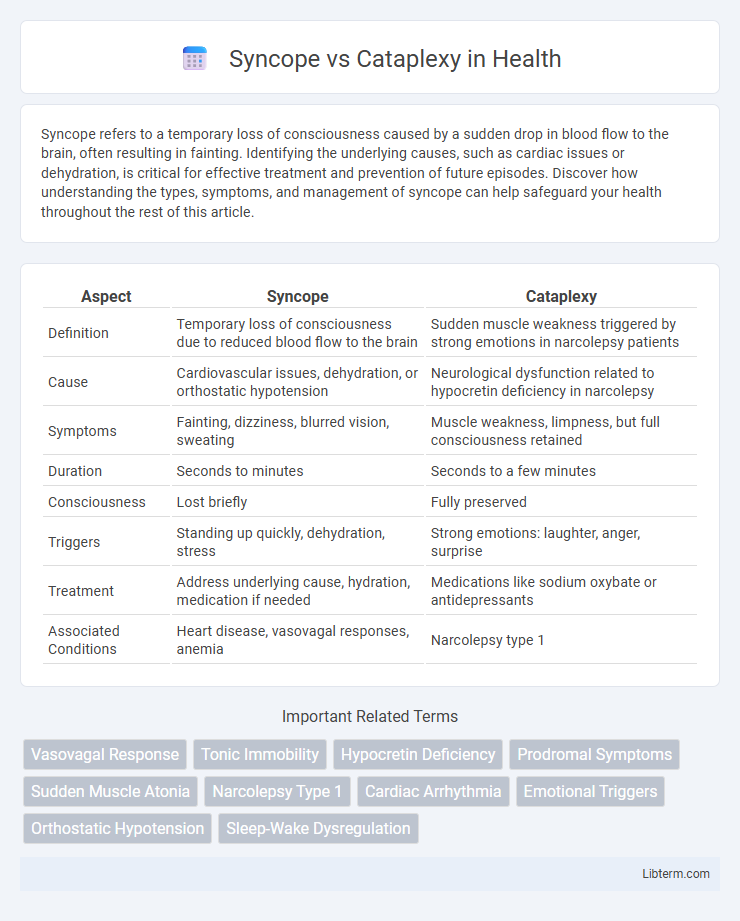
| Aspect | Syncope | Cataplexy |
|---|---|---|
| Definition | Temporary loss of consciousness due to reduced blood flow to the brain | Sudden muscle weakness triggered by strong emotions in narcolepsy patients |
| Cause | Cardiovascular issues, dehydration, or orthostatic hypotension | Neurological dysfunction related to hypocretin deficiency in narcolepsy |
| Symptoms | Fainting, dizziness, blurred vision, sweating | Muscle weakness, limpness, but full consciousness retained |
| Duration | Seconds to minutes | Seconds to a few minutes |
| Consciousness | Lost briefly | Fully preserved |
| Triggers | Standing up quickly, dehydration, stress | Strong emotions: laughter, anger, surprise |
| Treatment | Address underlying cause, hydration, medication if needed | Medications like sodium oxybate or antidepressants |
| Associated Conditions | Heart disease, vasovagal responses, anemia | Narcolepsy type 1 |
Introduction to Syncope and Cataplexy
Syncope refers to a sudden, temporary loss of consciousness caused by a drop in blood flow to the brain, often triggered by factors such as dehydration, low blood pressure, or cardiac issues. Cataplexy involves abrupt muscle weakness triggered by strong emotions, frequently associated with narcolepsy, a chronic neurological disorder affecting the brain's ability to regulate sleep-wake cycles. Differentiating syncope and cataplexy is crucial for accurate diagnosis and treatment, as they affect distinct physiological systems with different underlying causes.
Defining Syncope: Causes and Triggers
Syncope is a sudden, temporary loss of consciousness caused by a reduction in cerebral blood flow, often triggered by factors such as dehydration, stress, or standing for prolonged periods. Common causes include vasovagal syncope, orthostatic hypotension, cardiac arrhythmias, and structural heart disease. Identifying specific triggers like emotional distress, pain, or medication use is crucial for accurate diagnosis and management.
Understanding Cataplexy: Hallmarks and Risk Factors
Cataplexy is characterized by sudden, transient muscle weakness triggered by strong emotions such as laughter or anger, distinguishing it from syncope, which involves temporary loss of consciousness due to reduced blood flow to the brain. Key hallmarks include preserved consciousness during episodes, rapid onset, and brief duration, often associated with narcolepsy type 1. Risk factors for cataplexy involve genetic predisposition, particularly HLA-DQB1*06:02 allele, and abnormalities in hypocretin (orexin) neurotransmission within the hypothalamus.
Key Differences between Syncope and Cataplexy
Syncope is a temporary loss of consciousness caused by a sudden drop in blood flow to the brain, often triggered by factors like dehydration, low blood pressure, or cardiac issues. Cataplexy involves sudden muscle weakness or paralysis triggered by strong emotions such as laughter or surprise, and is closely associated with narcolepsy type 1. Unlike syncope, cataplexy does not involve loss of consciousness and is primarily a neurological disorder linked to hypocretin deficiency in the brain.
Clinical Presentation: Symptoms Comparison
Syncope presents as a sudden, transient loss of consciousness caused by cerebral hypoperfusion, often preceded by lightheadedness, dizziness, or visual disturbances, with rapid recovery once supine. Cataplexy involves abrupt, temporary muscle weakness triggered by strong emotions such as laughter or surprise, while maintaining full consciousness and awareness throughout the episode. Unlike syncope, cataplexy episodes do not cause loss of consciousness or autonomic symptoms like palpitations or sweating.
Pathophysiology: What Happens in the Body?
Syncope occurs due to a transient reduction in cerebral blood flow, often caused by factors such as vasodilation, bradycardia, or decreased cardiac output, leading to temporary loss of consciousness. Cataplexy involves sudden muscle weakness triggered by emotional stimuli, resulting from abnormal activation of the limbic system and dysfunction in hypothalamic hypocretin (orexin) production, which disrupts normal muscle tone regulation. While syncope relates to cardiovascular and autonomic nervous system disturbances, cataplexy stems from neurochemical imbalances affecting motor neuron control during wakefulness.
Diagnostic Approaches for Syncope vs Cataplexy
Diagnostic approaches for syncope primarily involve cardiovascular evaluations such as ECG, tilt-table testing, and Holter monitoring to detect arrhythmias or orthostatic hypotension. In contrast, cataplexy diagnosis relies heavily on clinical history, often accompanied by polysomnography and multiple sleep latency testing to confirm narcolepsy type 1. Accurate differentiation is crucial, as syncope indicates transient cerebral hypoperfusion, whereas cataplexy is characterized by sudden muscle atonia triggered by emotions.
Treatment and Management Strategies
Syncope treatment primarily involves identifying and addressing underlying causes such as dehydration, cardiac issues, or orthostatic hypotension, with strategies including fluid intake, medications, and lifestyle adjustments to prevent recurrence. Cataplexy management centers on pharmacological approaches like sodium oxybate, antidepressants (SSRIs or SNRIs), and lifestyle modifications to reduce trigger exposure and improve symptom control. Both conditions benefit from patient education and individualized care plans to optimize quality of life and minimize symptom episodes.
Prognosis and Long-Term Outlook
Syncope typically has a favorable prognosis with many cases resolving through lifestyle modifications and treatment of underlying causes, though recurrent episodes may increase the risk of injury. Cataplexy, often associated with narcolepsy type 1, is a chronic condition with a variable long-term outlook influenced by effective symptom management through medications like sodium oxybate or antidepressants. Both conditions require ongoing medical evaluation to optimize quality of life and reduce complications.
When to Seek Medical Attention
Seek immediate medical attention for syncope if episodes are frequent, prolonged, or accompanied by chest pain, palpitations, or neurological symptoms like weakness or confusion, as these may indicate underlying cardiac or neurological conditions. Cataplexy requires prompt evaluation when sudden muscle weakness occurs triggered by strong emotions, especially if episodes interfere with daily activities or are associated with other narcolepsy symptoms such as excessive daytime sleepiness. Early diagnosis and treatment are crucial to managing these conditions and preventing complications related to cardiovascular risks or compromised airway protection during cataplexy episodes.
Syncope Infographic
 libterm.com
libterm.com