Pulmonary embolism is a sudden blockage in a lung artery, usually caused by a blood clot traveling from the legs or other parts of the body. This serious condition can cause shortness of breath, chest pain, and even life-threatening complications if not treated promptly. Discover essential information about symptoms, risk factors, and treatment options to protect your health in the rest of this article.
Table of Comparison
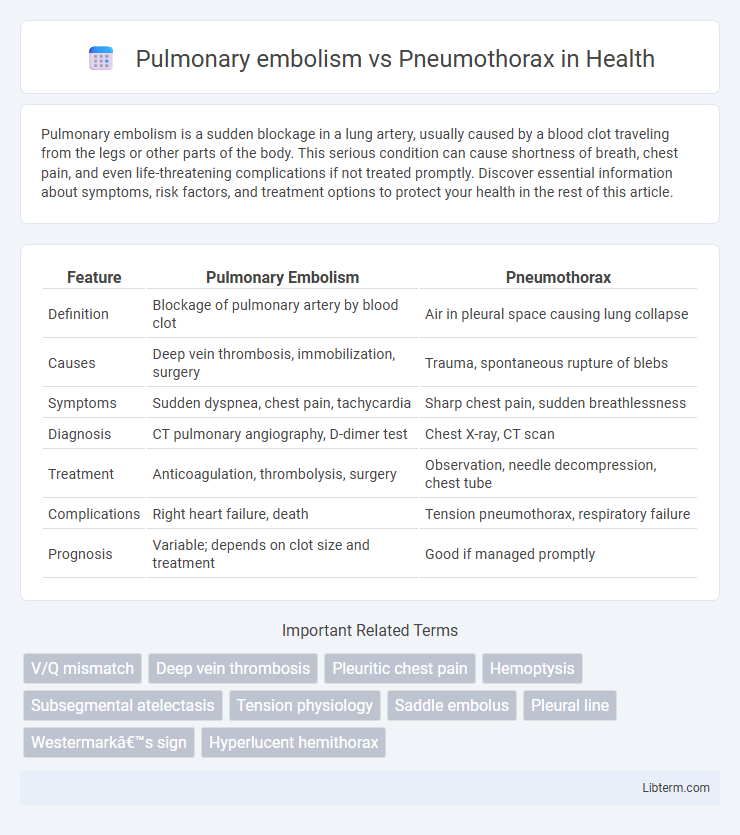
| Feature | Pulmonary Embolism | Pneumothorax |
|---|---|---|
| Definition | Blockage of pulmonary artery by blood clot | Air in pleural space causing lung collapse |
| Causes | Deep vein thrombosis, immobilization, surgery | Trauma, spontaneous rupture of blebs |
| Symptoms | Sudden dyspnea, chest pain, tachycardia | Sharp chest pain, sudden breathlessness |
| Diagnosis | CT pulmonary angiography, D-dimer test | Chest X-ray, CT scan |
| Treatment | Anticoagulation, thrombolysis, surgery | Observation, needle decompression, chest tube |
| Complications | Right heart failure, death | Tension pneumothorax, respiratory failure |
| Prognosis | Variable; depends on clot size and treatment | Good if managed promptly |
Overview of Pulmonary Embolism
Pulmonary embolism (PE) is a serious condition characterized by the sudden blockage of a pulmonary artery, usually due to a blood clot originating from deep vein thrombosis in the legs. Unlike pneumothorax, which involves air leakage into the pleural space causing lung collapse, PE impairs blood flow to lung tissue, leading to impaired gas exchange and potential respiratory failure. Early diagnosis using D-dimer testing, CT pulmonary angiography, and anticoagulant therapy is critical to reduce mortality associated with pulmonary embolism.
Overview of Pneumothorax
Pneumothorax is a condition characterized by the presence of air in the pleural space, leading to lung collapse and impaired respiratory function. It is classified into spontaneous, traumatic, and tension types, each varying in etiology and severity, with spontaneous pneumothorax often occurring in tall, thin individuals or those with underlying lung disease. Diagnosis is confirmed through chest X-ray or CT scan, while treatment ranges from observation and oxygen therapy to needle decompression or chest tube insertion based on the size and symptoms.
Causes and Risk Factors
Pulmonary embolism primarily results from the obstruction of pulmonary arteries by blood clots originating from deep vein thrombosis, with risk factors including prolonged immobility, surgery, cancer, and clotting disorders. Pneumothorax occurs due to air entering the pleural space, often caused by trauma, underlying lung diseases such as chronic obstructive pulmonary disease (COPD), or spontaneous rupture of blebs in healthy individuals. Smoking, tall stature, and previous episodes increase the risk of pneumothorax, whereas immobility, recent surgery, and genetic predispositions intensify the likelihood of pulmonary embolism.
Clinical Presentation and Symptoms
Pulmonary embolism typically presents with sudden onset dyspnea, pleuritic chest pain, tachypnea, and hypoxia, often accompanied by signs of deep vein thrombosis such as unilateral leg swelling. Pneumothorax manifests with acute unilateral pleuritic chest pain, respiratory distress, decreased or absent breath sounds on the affected side, and hyperresonance on percussion. Both conditions may show tachycardia and low oxygen saturation but differ in clinical signs like leg edema in pulmonary embolism versus tracheal deviation in tension pneumothorax.
Key Differences in Pathophysiology
Pulmonary embolism occurs when a blood clot obstructs pulmonary arteries, leading to impaired blood flow and ventilation-perfusion mismatch, causing hypoxemia and increased pulmonary artery pressure. Pneumothorax involves the accumulation of air in the pleural space, resulting in lung collapse and disrupted alveolar expansion, which compromises gas exchange. Unlike pulmonary embolism's vascular obstruction, pneumothorax is primarily a mechanical failure of lung expansion due to pleural injury or rupture.
Diagnostic Approaches
Pulmonary embolism diagnosis primarily relies on computed tomography pulmonary angiography (CTPA), D-dimer testing, and ventilation-perfusion (V/Q) scans to detect blood clots in pulmonary arteries. Pneumothorax diagnosis is predominantly confirmed using chest X-rays and point-of-care ultrasound, which reveal air presence in the pleural space causing lung collapse. Both conditions may warrant arterial blood gas analysis to assess oxygenation and ventilation status, guiding urgent clinical management.
Imaging Findings: PE vs Pneumothorax
Pulmonary embolism imaging primarily relies on CT pulmonary angiography, which reveals filling defects in the pulmonary arteries indicating vessel obstruction. In contrast, pneumothorax is diagnosed via chest X-ray or CT scan showing a visible pleural line with absent lung markings beyond the line, signifying air in the pleural space. While PE findings focus on vascular blockage, pneumothorax imaging highlights lung collapse and pleural air accumulation.
Emergency Management Strategies
Emergency management of pulmonary embolism prioritizes rapid anticoagulation with heparin to prevent clot propagation, alongside thrombolytic therapy in massive embolism cases to restore pulmonary perfusion. In contrast, pneumothorax treatment demands immediate needle decompression or chest tube insertion to evacuate intrapleural air and re-expand the lung, preventing tension physiology. Both conditions require continuous monitoring of respiratory status and hemodynamics to tailor interventions and prevent respiratory failure.
Short-term and Long-term Complications
Pulmonary embolism can cause short-term complications such as acute respiratory distress, right ventricular failure, and hypoxemia, while long-term complications include chronic thromboembolic pulmonary hypertension and recurrent embolic events. Pneumothorax often leads to acute respiratory compromise and lung collapse as short-term issues, with long-term risks involving persistent air leaks, pleural thickening, and potential development of fibrothorax or recurrent pneumothorax. Both conditions require prompt diagnosis and management to minimize morbidity and mortality associated with these respiratory emergencies.
Prevention and Patient Education
Effective prevention of pulmonary embolism includes early mobilization after surgery, use of anticoagulants, and compression stockings to reduce venous thromboembolism risk. Pneumothorax prevention emphasizes avoiding high-risk activities such as smoking cessation, proper management of underlying lung diseases, and careful use of mechanical ventilation in vulnerable patients. Patient education should highlight recognizing early symptoms like sudden chest pain and shortness of breath, promoting timely medical intervention to reduce complications from both conditions.
Pulmonary embolism Infographic
 libterm.com
libterm.com