Hyperoxemia occurs when there is an excessive amount of oxygen in the blood, often due to high oxygen therapy or exposure to pure oxygen environments. This condition can lead to oxygen toxicity, causing symptoms like lung damage, vision problems, or neurological disturbances. Explore the article to understand hyperoxemia's causes, risks, and management strategies for your health.
Table of Comparison
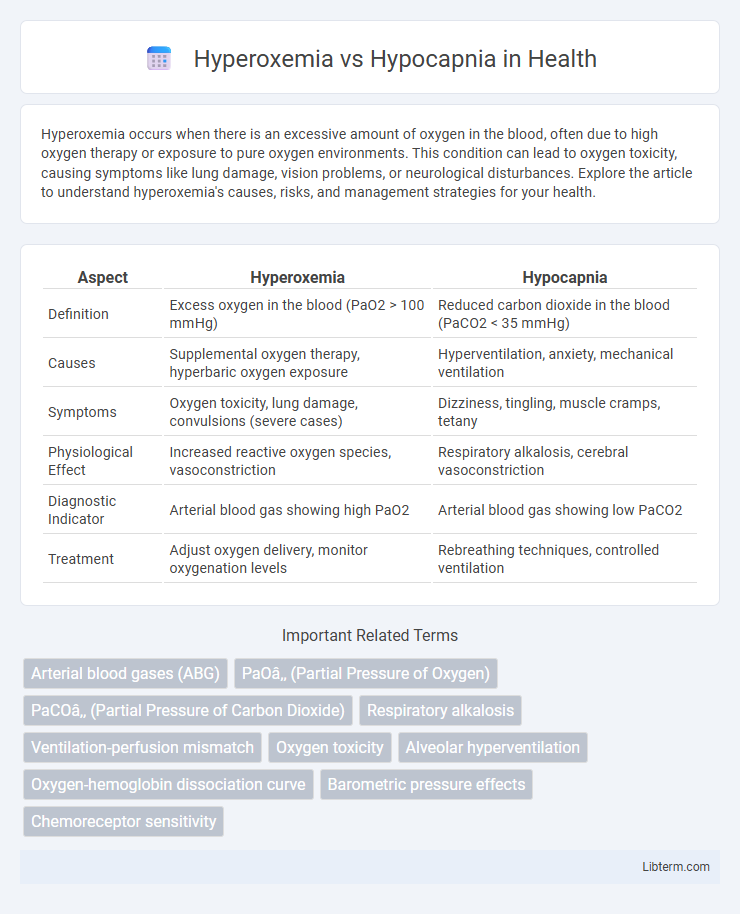
| Aspect | Hyperoxemia | Hypocapnia |
|---|---|---|
| Definition | Excess oxygen in the blood (PaO2 > 100 mmHg) | Reduced carbon dioxide in the blood (PaCO2 < 35 mmHg) |
| Causes | Supplemental oxygen therapy, hyperbaric oxygen exposure | Hyperventilation, anxiety, mechanical ventilation |
| Symptoms | Oxygen toxicity, lung damage, convulsions (severe cases) | Dizziness, tingling, muscle cramps, tetany |
| Physiological Effect | Increased reactive oxygen species, vasoconstriction | Respiratory alkalosis, cerebral vasoconstriction |
| Diagnostic Indicator | Arterial blood gas showing high PaO2 | Arterial blood gas showing low PaCO2 |
| Treatment | Adjust oxygen delivery, monitor oxygenation levels | Rebreathing techniques, controlled ventilation |
Introduction to Hyperoxemia and Hypocapnia
Hyperoxemia refers to an elevated level of oxygen in the blood, typically measured by arterial oxygen partial pressure (PaO2) exceeding 100 mmHg, and can result from supplemental oxygen therapy or hyperbaric oxygen exposure. Hypocapnia is characterized by reduced arterial carbon dioxide partial pressure (PaCO2) below 35 mmHg, often due to hyperventilation or respiratory alkalosis. Both conditions significantly affect respiratory physiology by altering gas exchange and acid-base balance, necessitating careful monitoring in clinical settings such as intensive care units.
Understanding Blood Gas Imbalances
Hyperoxemia, characterized by excess oxygen in the blood, can lead to oxidative stress and tissue damage, while hypocapnia involves reduced carbon dioxide levels, often causing respiratory alkalosis and altered blood pH. Monitoring arterial blood gases (ABGs) is crucial for detecting these imbalances, as hyperoxemia shifts oxygen saturation curves and hypocapnia affects CO2 partial pressure (PaCO2). Effective management requires precise titration of oxygen therapy and ventilation adjustments to maintain homeostasis and prevent complications in respiratory function.
Causes of Hyperoxemia
Hyperoxemia, characterized by elevated oxygen levels in the blood, commonly results from excessive supplemental oxygen administration, underlying lung diseases such as chronic obstructive pulmonary disease (COPD), or hyperbaric oxygen therapy. It occurs when the partial pressure of oxygen (PaO2) exceeds normal physiological levels, often surpassing 100 mmHg. Understanding these causes is critical to prevent oxygen toxicity and maintain optimal respiratory function.
Causes of Hypocapnia
Hypocapnia, characterized by reduced carbon dioxide levels in the blood, commonly results from hyperventilation caused by anxiety, pain, or respiratory disorders such as asthma and chronic obstructive pulmonary disease (COPD). Other causes include metabolic conditions like sepsis or fever, leading to increased respiratory rate and excessive CO2 expulsion. This contrasts with hyperoxemia, marked by elevated oxygen levels, which primarily arises from supplemental oxygen therapy or high atmospheric oxygen exposure.
Clinical Manifestations of Hyperoxemia
Hyperoxemia presents clinically with symptoms including visual disturbances, confusion, nausea, and muscle twitching due to excessive oxygen levels in arterial blood. Pulmonary effects such as absorption atelectasis and oxidative lung injury may manifest with dyspnea and chest discomfort. Prolonged hyperoxemia increases the risk of oxygen toxicity, which can lead to seizures and central nervous system complications.
Clinical Manifestations of Hypocapnia
Hypocapnia, characterized by reduced arterial carbon dioxide levels (PaCO2 < 35 mmHg), commonly manifests with symptoms such as dizziness, paresthesia, muscle cramps, and tetany due to respiratory alkalosis-induced cerebral vasoconstriction. Clinical signs also include carpopedal spasms and prolonged QT interval on electrocardiogram, often accompanying hyperventilation syndrome or anxiety attacks. Identification of hypocapnia is critical in differentiating it from hyperoxemia, which primarily involves elevated oxygen levels rather than altered carbon dioxide homeostasis.
Diagnostic Approaches for Blood Gas Abnormalities
Diagnostic approaches for hyperoxemia and hypocapnia primarily involve arterial blood gas (ABG) analysis to assess oxygen and carbon dioxide levels accurately. Hyperoxemia is identified by elevated partial pressure of oxygen (PaO2) above 100 mmHg, often caused by excessive oxygen therapy, while hypocapnia is characterized by decreased partial pressure of carbon dioxide (PaCO2) below 35 mmHg, typically resulting from hyperventilation. Continuous monitoring through pulse oximetry and capnography complements ABG to provide real-time data, aiding in the precise diagnosis and management of these blood gas abnormalities.
Complications Associated with Hyperoxemia and Hypocapnia
Hyperoxemia can induce oxidative stress leading to cellular damage, lung injury, and impaired vasoregulation, increasing the risk of acute respiratory distress syndrome (ARDS) and worsening outcomes in critically ill patients. Hypocapnia often causes cerebral vasoconstriction, reducing cerebral blood flow and potentially resulting in dizziness, seizures, or ischemic brain injury in severe cases. Both conditions disrupt homeostasis, necessitating careful monitoring of arterial blood gases to avoid complications during respiratory therapy.
Treatment Strategies and Management
Treatment strategies for hyperoxemia focus on reducing oxygen delivery to prevent oxidative stress and lung injury by titrating supplemental oxygen to maintain target saturation levels, generally between 90-96%. Management of hypocapnia involves addressing underlying causes such as hyperventilation syndrome or respiratory alkalosis, often using controlled breathing techniques, rebreathing methods, or adjusting ventilator settings to increase carbon dioxide levels safely. Both conditions require continuous monitoring of arterial blood gases and patient symptoms to optimize oxygen and carbon dioxide balance for homeostasis.
Prevention and Monitoring Recommendations
Preventing hyperoxemia involves maintaining targeted oxygen saturation levels between 92-96% using controlled oxygen delivery devices to avoid oxygen toxicity. Monitoring arterial blood gases and pulse oximetry is critical for early detection of hypocapnia, with frequent adjustments to ventilation settings in mechanically ventilated patients to prevent excessive CO2 elimination. Continuous capnography and regular assessment of respiratory rate and depth allow timely intervention to maintain normocapnia and prevent associated complications.
Hyperoxemia Infographic
 libterm.com
libterm.com