Uremia occurs when the kidneys are unable to remove waste products from the blood, leading to a dangerous buildup of toxins that can affect multiple organs. Symptoms may include fatigue, nausea, confusion, and in severe cases, seizures or coma. Discover more about the causes, symptoms, and treatments to protect your health by reading the full article.
Table of Comparison
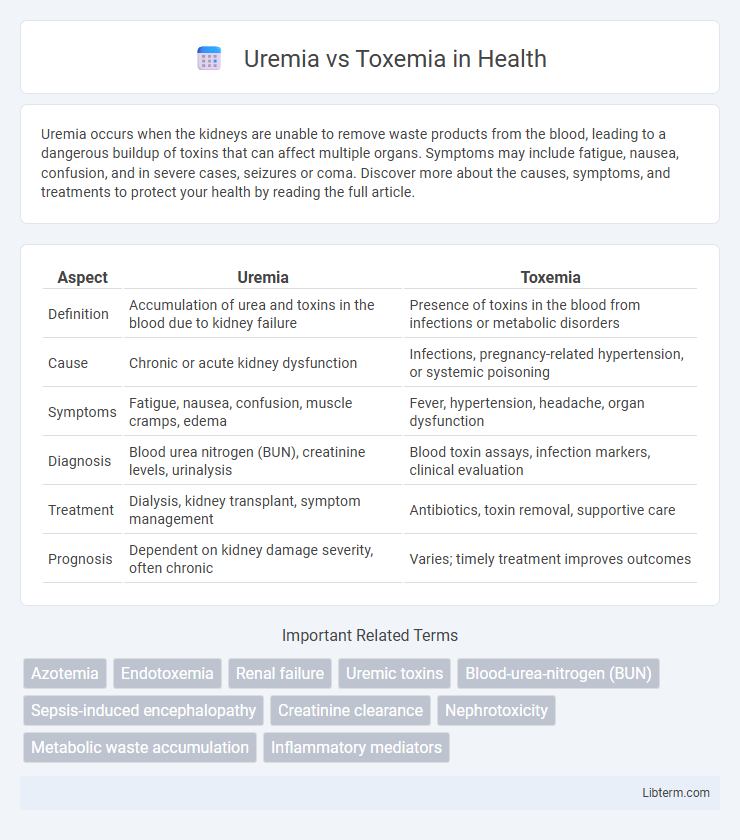
| Aspect | Uremia | Toxemia |
|---|---|---|
| Definition | Accumulation of urea and toxins in the blood due to kidney failure | Presence of toxins in the blood from infections or metabolic disorders |
| Cause | Chronic or acute kidney dysfunction | Infections, pregnancy-related hypertension, or systemic poisoning |
| Symptoms | Fatigue, nausea, confusion, muscle cramps, edema | Fever, hypertension, headache, organ dysfunction |
| Diagnosis | Blood urea nitrogen (BUN), creatinine levels, urinalysis | Blood toxin assays, infection markers, clinical evaluation |
| Treatment | Dialysis, kidney transplant, symptom management | Antibiotics, toxin removal, supportive care |
| Prognosis | Dependent on kidney damage severity, often chronic | Varies; timely treatment improves outcomes |
Understanding Uremia: Definition and Causes
Uremia is a clinical syndrome resulting from the accumulation of nitrogenous waste products in the blood due to impaired kidney function, particularly in chronic kidney disease or acute renal failure. It is characterized by elevated blood urea nitrogen (BUN) and creatinine levels, leading to toxic effects on multiple organ systems. Unlike toxemia, which involves the presence of toxins from infections in the bloodstream, uremia specifically arises from renal insufficiency and the inability to excrete waste metabolites.
Exploring Toxemia: What It Means
Toxemia refers to the presence of toxins in the blood, often resulting from infections or metabolic imbalances, whereas uremia specifically denotes the accumulation of urea and other nitrogenous waste products due to kidney failure. In toxemia, harmful substances produced by bacteria or disrupted metabolic processes enter the bloodstream, causing systemic toxicity. Understanding toxemia involves recognizing its role in conditions like preeclampsia and sepsis, where toxin buildup leads to widespread inflammation and organ dysfunction.
Key Differences Between Uremia and Toxemia
Uremia is a condition characterized by elevated blood urea nitrogen levels and impaired kidney function, whereas toxemia refers to the presence of toxins in the blood, often related to infections or pregnancy complications. Uremia primarily results from chronic kidney disease or acute kidney failure, leading to the accumulation of waste products, while toxemia involves systemic toxicity affecting multiple organ systems. Diagnostic markers for uremia include high creatinine and urea levels, whereas toxemia diagnosis relies on identifying specific toxins or signs of infection and inflammation in the bloodstream.
Major Causes: Uremia vs Toxemia
Uremia primarily results from chronic kidney failure, leading to the accumulation of nitrogenous waste products like urea in the blood due to impaired renal filtration. Toxemia arises from the presence of toxins in the bloodstream, commonly caused by infections such as bacterial sepsis or pregnancy-related conditions like preeclampsia. Differentiating these conditions involves understanding the underlying pathology: uremia's renal origin versus toxemia's systemic infectious or inflammatory etiology.
Clinical Symptoms and Manifestations
Uremia presents with clinical symptoms such as fatigue, anorexia, nausea, vomiting, and mental confusion due to the accumulation of nitrogenous waste products in the blood from renal failure. Toxemia, often seen in pregnancy as preeclampsia, manifests with hypertension, proteinuria, edema, and headache caused by abnormal toxin buildup affecting vascular functions. Both conditions exhibit systemic effects, but uremia primarily reflects kidney dysfunction while toxemia involves multisystem vascular disturbances.
Diagnostic Approaches for Both Conditions
Diagnostic approaches for uremia primarily involve blood tests measuring elevated blood urea nitrogen (BUN) and serum creatinine levels to assess impaired kidney function. In contrast, toxemia diagnosis often requires identifying specific toxins or toxins' effects through blood and urine analysis, alongside clinical evaluation of symptoms such as hypertension and proteinuria, especially in pregnancy-related toxemia (pre-eclampsia). Imaging studies and renal function tests support differentiation by evaluating organ damage severity and underlying causes.
Treatment Strategies: A Comparative Overview
Uremia treatment primarily involves dialysis to remove waste products and toxins from the blood in cases of severe kidney failure, along with dietary modifications and management of electrolyte imbalances. Toxemia, often related to conditions like preeclampsia, requires interventions such as blood pressure control, bed rest, and in severe cases, early delivery of the fetus to prevent maternal and fetal complications. Both conditions necessitate close monitoring and supportive care tailored to the underlying cause to optimize patient outcomes.
Potential Complications and Risks
Uremia, resulting from kidney failure, poses risks such as severe electrolyte imbalances, pericarditis, and encephalopathy due to toxin accumulation in the blood. Toxemia, often related to pregnancy or infections, can lead to preeclampsia, eclampsia, and multi-organ dysfunction if untreated. Both conditions require prompt medical intervention to prevent life-threatening complications including cardiovascular collapse and irreversible organ damage.
Preventive Measures for Uremia and Toxemia
Preventive measures for uremia primarily involve managing chronic kidney disease through regular monitoring of kidney function, maintaining blood pressure within target ranges, and avoiding nephrotoxic substances such as NSAIDs and excess protein intake. Toxemia prevention focuses on addressing underlying causes like infections, sepsis, or metabolic imbalances by promoting early detection, adequate hydration, and prompt medical treatment to eliminate toxins and reduce systemic inflammation. Both conditions benefit from lifestyle modifications, including balanced nutrition, controlled blood glucose levels, and routine medical evaluations to prevent progression and complications.
Prognosis and Long-Term Outcomes
Uremia, resulting from chronic kidney failure, typically has a poorer prognosis with increased risk of complications like cardiovascular disease and neurological impairment, leading to progressive decline without dialysis or transplant. Toxemia, often associated with pregnancy-related conditions such as preeclampsia, generally resolves after delivery, but severe cases can cause long-term maternal hypertension or organ damage. Long-term outcomes for uremia heavily depend on timely renal replacement therapy, whereas toxemia's prognosis improves significantly with early diagnosis and management.
Uremia Infographic
 libterm.com
libterm.com