Cholestasis occurs when bile flow from the liver is reduced or blocked, leading to the buildup of bile acids in the liver and bloodstream, which can cause itching, jaundice, and liver damage. Identifying the underlying cause, such as gallstones, infections, or liver disease, is crucial for effective treatment and preventing complications. Explore the full article to understand symptoms, causes, and management strategies to protect your liver health.
Table of Comparison
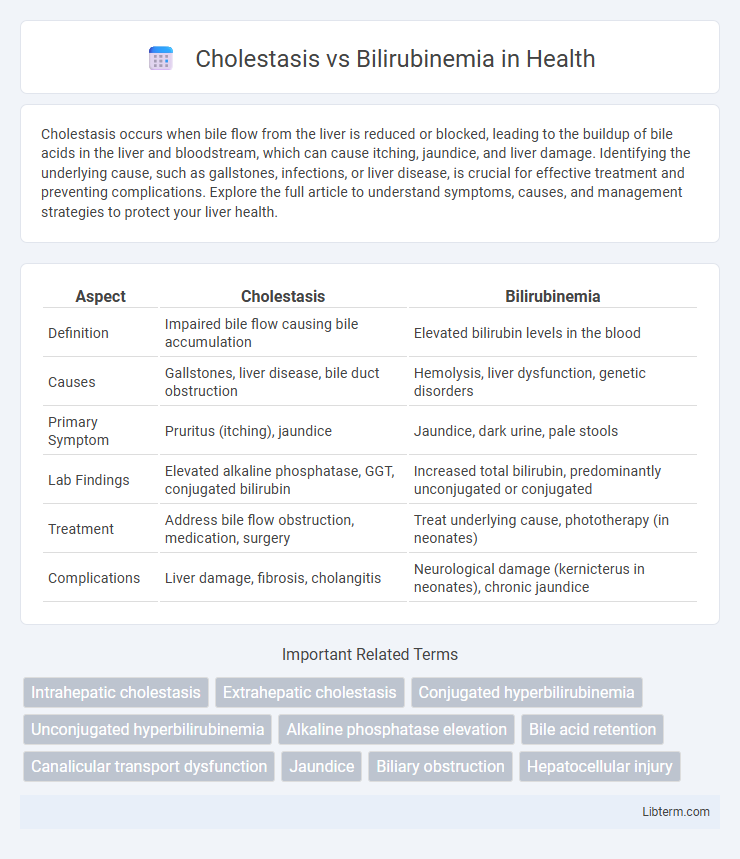
| Aspect | Cholestasis | Bilirubinemia |
|---|---|---|
| Definition | Impaired bile flow causing bile accumulation | Elevated bilirubin levels in the blood |
| Causes | Gallstones, liver disease, bile duct obstruction | Hemolysis, liver dysfunction, genetic disorders |
| Primary Symptom | Pruritus (itching), jaundice | Jaundice, dark urine, pale stools |
| Lab Findings | Elevated alkaline phosphatase, GGT, conjugated bilirubin | Increased total bilirubin, predominantly unconjugated or conjugated |
| Treatment | Address bile flow obstruction, medication, surgery | Treat underlying cause, phototherapy (in neonates) |
| Complications | Liver damage, fibrosis, cholangitis | Neurological damage (kernicterus in neonates), chronic jaundice |
Introduction to Cholestasis and Bilirubinemia
Cholestasis refers to the impairment or cessation of bile flow from the liver, leading to the accumulation of bile acids in the liver and bloodstream, which can cause jaundice and liver damage. Bilirubinemia is characterized by elevated levels of bilirubin in the blood, often manifesting as jaundice and indicating underlying liver dysfunction or hemolytic processes. Understanding the distinct pathophysiological mechanisms of cholestasis and bilirubinemia is essential for accurate diagnosis and targeted treatment strategies in hepatic disorders.
Understanding Cholestasis: Definition and Causes
Cholestasis is a condition characterized by impaired bile flow from the liver to the duodenum, leading to bile accumulation and subsequent liver dysfunction. Its causes include intrahepatic factors such as viral hepatitis, primary biliary cholangitis, and drug-induced liver injury, as well as extrahepatic obstructions like gallstones, tumors, or strictures in the bile ducts. This bile flow disruption results in elevated serum levels of bile acids and conjugated bilirubin, distinguishing it from bilirubinemia, which specifically refers to increased bilirubin concentration in the blood due to various hemolytic or hepatic disorders.
What is Bilirubinemia? Overview and Etiology
Bilirubinemia refers to an elevated level of bilirubin in the blood, typically resulting from excessive breakdown of red blood cells or impaired bilirubin metabolism. Common causes include hemolytic anemias, liver dysfunction, and genetic disorders such as Gilbert's syndrome or Crigler-Najjar syndrome. This condition can lead to jaundice and requires careful evaluation to determine the underlying etiology and appropriate treatment.
Key Pathophysiological Differences
Cholestasis involves impaired bile flow leading to accumulation of bile acids, bilirubin, and cholesterol in the liver, causing hepatocellular damage and cholestatic jaundice. Bilirubinemia specifically refers to elevated bilirubin levels in the blood, resulting from increased bilirubin production, decreased conjugation, or impaired excretion, manifesting as prehepatic, hepatic, or posthepatic jaundice. The key pathophysiological difference lies in cholestasis primarily disrupting bile secretion and transport, whereas bilirubinemia centers on bilirubin metabolism abnormalities affecting its serum concentration.
Signs and Symptoms: Cholestasis vs Bilirubinemia
Cholestasis often presents with pruritus, dark urine, pale stools, and jaundice due to impaired bile flow, while bilirubinemia primarily manifests as jaundice with yellowing of the skin and sclera from elevated bilirubin levels. Patients with cholestasis may also experience fatigue and abdominal discomfort, whereas bilirubinemia without cholestasis usually lacks pruritus and pale stools. Laboratory findings in cholestasis show elevated alkaline phosphatase and gamma-glutamyl transferase, whereas bilirubinemia mainly demonstrates increased total and direct bilirubin concentrations.
Diagnostic Approaches and Laboratory Markers
Cholestasis is primarily diagnosed through elevated serum alkaline phosphatase (ALP) and gamma-glutamyl transferase (GGT) levels, while bilirubinemia is characterized by increased total and direct bilirubin concentrations in blood tests. Imaging modalities such as ultrasound, MRCP, or ERCP aid in identifying bile duct obstruction in cholestasis, whereas bilirubinemia evaluation focuses on distinguishing between conjugated and unconjugated hyperbilirubinemia using fractionated bilirubin levels. Liver function tests, including AST and ALT, along with clinical presentation, further support differential diagnosis by revealing hepatocellular versus cholestatic patterns of liver injury.
Underlying Diseases Associated with Each Condition
Cholestasis is often associated with underlying diseases such as primary biliary cholangitis, primary sclerosing cholangitis, and bile duct obstruction from gallstones or tumors, leading to impaired bile flow. Bilirubinemia, characterized by elevated bilirubin levels, is commonly linked to hemolytic anemias, liver dysfunctions such as hepatitis or cirrhosis, and genetic conditions like Gilbert's syndrome. The differentiation in underlying diseases is crucial for targeted diagnosis and treatment of cholestasis versus bilirubinemia.
Treatment Options: Management Strategies
Treatment options for cholestasis primarily involve addressing the underlying cause, such as using ursodeoxycholic acid to improve bile flow and reduce liver damage, while managing symptoms like itching with antihistamines or rifampicin. In cases of bilirubinemia, management depends on the type; unconjugated hyperbilirubinemia often requires phototherapy or exchange transfusion in severe neonatal jaundice, whereas conjugated hyperbilirubinemia treatment targets the specific liver or bile duct pathology. Both conditions may require supportive care, including nutritional support and monitoring for complications like liver fibrosis or encephalopathy.
Complications and Prognosis
Cholestasis often leads to complications such as pruritus, fat-soluble vitamin deficiencies, and progressive liver damage, which can result in cirrhosis or liver failure if untreated. Bilirubinemia primarily causes jaundice and, in severe neonatal cases, kernicterus, a neurological damage with potentially fatal outcomes. Prognosis depends on early diagnosis and management, with cholestasis requiring intervention to prevent bile duct injury and bilirubinemia needing timely reduction of bilirubin levels to avoid neurotoxicity.
Summary: Comparing Cholestasis and Bilirubinemia
Cholestasis is characterized by impaired bile flow leading to accumulation of bile acids and conjugated bilirubin, whereas bilirubinemia specifically refers to elevated levels of unconjugated or conjugated bilirubin in the blood. Both conditions cause jaundice, but cholestasis often involves symptoms like pruritus and pale stools due to bile salt retention, while bilirubinemia may arise from hemolysis or liver dysfunction without bile flow obstruction. Diagnostic differentiation relies on serum bilirubin fractions, liver enzyme patterns, and imaging to identify the underlying etiology for targeted management.
Cholestasis Infographic
 libterm.com
libterm.com