Cervical health plays a crucial role in maintaining overall well-being, as issues in this area can lead to significant discomfort and complications. Regular screenings and awareness of symptoms are essential for early detection and effective treatment. Explore the following article to understand how you can protect your cervical health and address potential concerns.
Table of Comparison
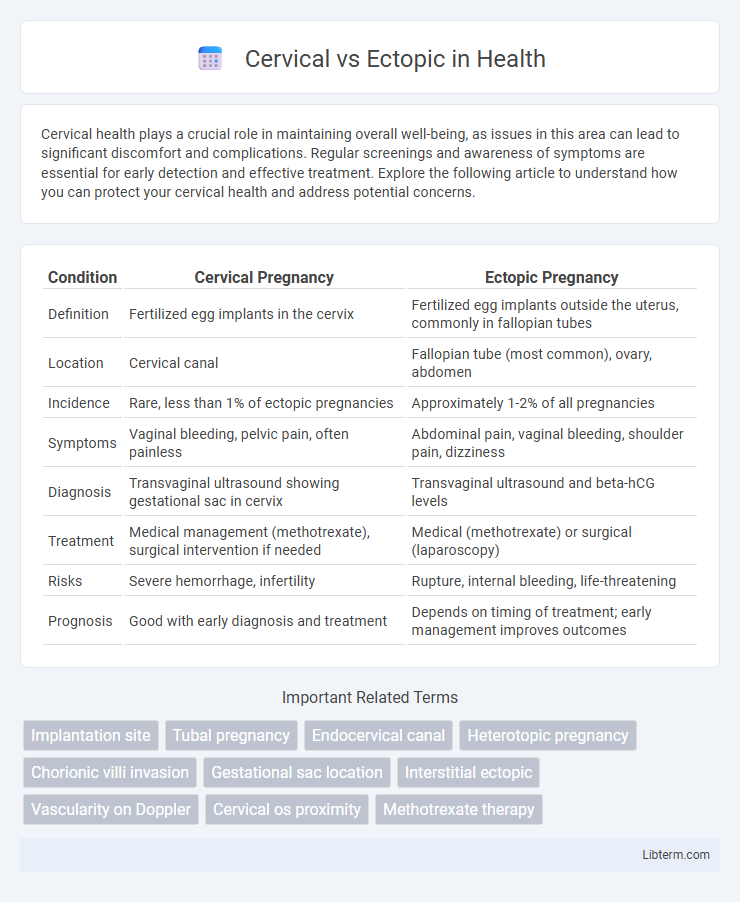
| Condition | Cervical Pregnancy | Ectopic Pregnancy |
|---|---|---|
| Definition | Fertilized egg implants in the cervix | Fertilized egg implants outside the uterus, commonly in fallopian tubes |
| Location | Cervical canal | Fallopian tube (most common), ovary, abdomen |
| Incidence | Rare, less than 1% of ectopic pregnancies | Approximately 1-2% of all pregnancies |
| Symptoms | Vaginal bleeding, pelvic pain, often painless | Abdominal pain, vaginal bleeding, shoulder pain, dizziness |
| Diagnosis | Transvaginal ultrasound showing gestational sac in cervix | Transvaginal ultrasound and beta-hCG levels |
| Treatment | Medical management (methotrexate), surgical intervention if needed | Medical (methotrexate) or surgical (laparoscopy) |
| Risks | Severe hemorrhage, infertility | Rupture, internal bleeding, life-threatening |
| Prognosis | Good with early diagnosis and treatment | Depends on timing of treatment; early management improves outcomes |
Overview: Cervical vs Ectopic Pregnancy
Cervical pregnancy is a rare type of ectopic pregnancy where the embryo implants within the cervical canal, while ectopic pregnancies more commonly occur in the fallopian tubes. Both conditions pose significant risks, including severe bleeding, but cervical pregnancies require distinct diagnostic and management approaches due to their unique location. Early ultrasound imaging is critical to differentiate cervical pregnancy from other forms of ectopic gestation to guide appropriate treatment and reduce maternal morbidity.
Key Differences in Location
Cervical and ectopic pregnancies differ primarily in their implantation sites; cervical pregnancies implant within the cervical canal, whereas ectopic pregnancies typically occur outside the uterine cavity, most commonly in the fallopian tubes. The cervical location is below the internal os, while ectopic sites can include tubal, ovarian, or abdominal regions. Accurate localization through ultrasound is critical for diagnosis and management due to the varying risks and treatment approaches associated with each site.
Causes and Risk Factors
Cervical pregnancy occurs when the fertilized egg implants in the cervix, often linked to previous cervical surgery, in vitro fertilization, or underlying uterine abnormalities. Ectopic pregnancy, predominantly tubal, arises from impaired embryo transport due to factors like pelvic inflammatory disease, previous ectopic pregnancies, or fallopian tube damage caused by infections or surgeries. Both conditions share risk factors including assisted reproductive techniques, smoking, and a history of pelvic infections, significantly affecting implantation sites and pregnancy viability.
Early Signs and Symptoms
Early signs of cervical pregnancy include vaginal bleeding, lower abdominal pain, and a soft, enlarged cervix on examination. Ectopic pregnancy symptoms typically involve sharp pelvic or abdominal pain, shoulder pain due to internal bleeding, and irregular vaginal spotting or bleeding. Prompt recognition of these symptoms is critical for early diagnosis and management to prevent complications.
Diagnostic Methods
Cervical pregnancy diagnosis primarily relies on transvaginal ultrasound, revealing a gestational sac within the cervical canal, often accompanied by an empty uterine cavity and a closed internal os. Doppler imaging enhances detection by identifying peritrophoblastic blood flow around the cervical gestational sac, distinguishing it from other conditions like miscarriages. In contrast, ectopic pregnancies outside the cervix, such as tubal ectopics, are diagnosed using a combination of serial serum beta-hCG levels and transvaginal ultrasound to locate the extrauterine gestational sac or identify adnexal masses.
Potential Health Complications
Cervical and ectopic pregnancies both pose serious potential health complications, including severe bleeding and increased risk of infection. Cervical pregnancy can lead to significant hemorrhage due to the rich vascular supply of the cervix, often necessitating medical intervention to prevent life-threatening blood loss. Ectopic pregnancy, commonly occurring in the fallopian tube, risks tubal rupture, which can cause internal bleeding, shock, and infertility if not promptly treated.
Treatment Options and Approaches
Treatment options for cervical ectopic pregnancy include systemic methotrexate administration, local injection of methotrexate or potassium chloride, and surgical interventions like curettage or hysterectomy depending on gestational age and hemodynamic stability. Ectopic pregnancies located outside the cervix, such as tubal ectopics, typically require laparoscopic salpingostomy or salpingectomy, while medical management with methotrexate remains an option for early, unruptured cases. Preservation of fertility, hemodynamic status, gestational age, and beta-hCG levels are critical factors guiding the selection of individualized treatment approaches in both cervical and other ectopic pregnancies.
Prognosis and Recovery
Cervical pregnancies generally have a better prognosis with timely diagnosis and treatment, leading to lower morbidity compared to ectopic pregnancies located outside the cervix such as tubal pregnancies. Ectopic pregnancies often carry higher risks of rupture and hemorrhage, resulting in more complex recovery and potential fertility complications. Recovery from cervical pregnancy typically involves less invasive procedures, whereas ectopic pregnancy treatment may require surgical intervention and longer recovery times due to tissue damage and potential complications.
Impact on Future Fertility
Cervical ectopic pregnancies are rare and often require conservative treatments to preserve fertility, although they pose risks of significant bleeding and complications. Ectopic pregnancies in locations other than the cervix, such as the fallopian tubes, commonly lead to tubal damage or removal, which can reduce future fertility and increase the risk of infertility. Early diagnosis and appropriate management are critical to minimizing reproductive consequences and improving the chances of successful future pregnancies.
Preventive Measures and Patient Guidance
Preventive measures for cervical pregnancy include early ultrasound screening and prompt diagnosis to avoid complications, while ectopic pregnancy prevention focuses on reducing risk factors such as pelvic inflammatory disease through safe sexual practices and timely treatment of infections. Patient guidance emphasizes awareness of symptoms like abnormal bleeding and pelvic pain, encouraging immediate medical consultation to ensure early intervention. Regular prenatal care and risk factor management are critical in minimizing adverse outcomes for both cervical and ectopic pregnancies.
Cervical Infographic
 libterm.com
libterm.com