Diabetes is a chronic condition characterized by high blood sugar levels due to the body's inability to produce or effectively use insulin. Managing your blood glucose through lifestyle changes, medication, and regular monitoring is crucial to prevent complications such as heart disease, nerve damage, and vision loss. Explore the rest of this article to learn effective strategies for controlling diabetes and improving your overall health.
Table of Comparison
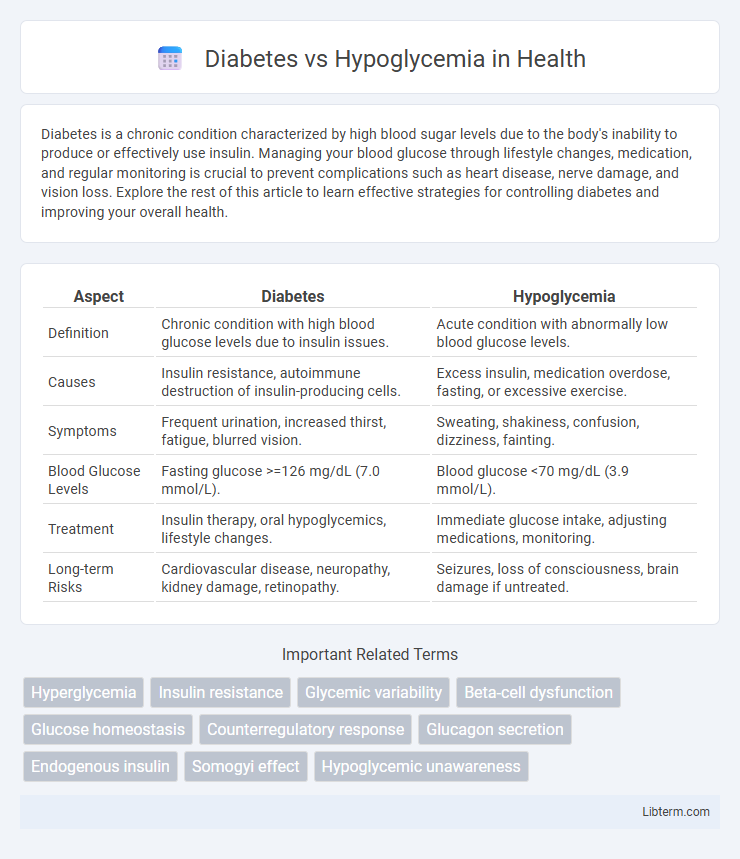
| Aspect | Diabetes | Hypoglycemia |
|---|---|---|
| Definition | Chronic condition with high blood glucose levels due to insulin issues. | Acute condition with abnormally low blood glucose levels. |
| Causes | Insulin resistance, autoimmune destruction of insulin-producing cells. | Excess insulin, medication overdose, fasting, or excessive exercise. |
| Symptoms | Frequent urination, increased thirst, fatigue, blurred vision. | Sweating, shakiness, confusion, dizziness, fainting. |
| Blood Glucose Levels | Fasting glucose >=126 mg/dL (7.0 mmol/L). | Blood glucose <70 mg/dL (3.9 mmol/L). |
| Treatment | Insulin therapy, oral hypoglycemics, lifestyle changes. | Immediate glucose intake, adjusting medications, monitoring. |
| Long-term Risks | Cardiovascular disease, neuropathy, kidney damage, retinopathy. | Seizures, loss of consciousness, brain damage if untreated. |
Understanding Diabetes and Hypoglycemia
Diabetes is a chronic metabolic disorder characterized by high blood glucose levels due to insulin deficiency or resistance, leading to symptoms like frequent urination, excessive thirst, and fatigue. Hypoglycemia, commonly a complication in people with diabetes, occurs when blood glucose levels drop below 70 mg/dL, causing symptoms such as shakiness, sweating, confusion, and in severe cases, loss of consciousness. Effective management of diabetes involves monitoring blood sugar levels and insulin therapy, while preventing hypoglycemia requires balancing medication, food intake, and physical activity.
Causes of Diabetes vs Hypoglycemia
Diabetes is primarily caused by insulin resistance or insufficient insulin production due to genetic factors, autoimmune destruction of pancreatic beta cells, or obesity-related metabolic dysfunction. Hypoglycemia often results from excessive insulin administration, prolonged fasting, certain medications, or hormonal imbalances affecting glucose regulation. Understanding the distinct causes of diabetes and hypoglycemia is essential for accurate diagnosis and effective treatment strategies.
Key Symptoms: Diabetes and Hypoglycemia
Diabetes is characterized by symptoms such as frequent urination, excessive thirst, unexplained weight loss, and persistent fatigue, resulting from high blood glucose levels. Hypoglycemia presents with symptoms including shakiness, sweating, confusion, irritability, and rapid heartbeat due to abnormally low blood sugar. Recognizing these key symptoms is critical for timely diagnosis and effective management of both conditions.
Diagnosis: How to Differentiate
Diabetes diagnosis primarily relies on fasting blood glucose levels above 126 mg/dL, HbA1c values exceeding 6.5%, and oral glucose tolerance tests, whereas hypoglycemia is identified by blood glucose levels below 70 mg/dL accompanied by symptoms like sweating, confusion, and tremors. Continuous glucose monitoring systems and patient symptom history help differentiate episodic hypoglycemia from chronic hyperglycemia seen in diabetes. Confirmatory tests such as insulin, C-peptide levels, and oral glucose tolerance tests assist clinicians in distinguishing insulinoma-induced hypoglycemia from diabetes mellitus.
Risk Factors and Triggers
Diabetes risk factors include obesity, sedentary lifestyle, family history, and age over 45, which contribute to insulin resistance and impaired glucose metabolism. Hypoglycemia triggers often involve excessive insulin dosage, skipped meals, intense physical activity, and alcohol consumption, leading to dangerously low blood sugar levels. Monitoring blood glucose and adjusting medication based on lifestyle factors are critical to managing both conditions effectively.
Blood Sugar Levels: Highs vs Lows
Diabetes is characterized by consistently high blood sugar levels due to insulin resistance or deficiency, leading to hyperglycemia, which can cause long-term complications like neuropathy and cardiovascular disease. Hypoglycemia occurs when blood sugar drops below normal levels, often under 70 mg/dL, causing symptoms such as shakiness, confusion, and in severe cases, seizures. Monitoring and managing glucose levels through medication, diet, and lifestyle adjustments are critical to preventing dangerous highs in diabetes and acute lows in hypoglycemia.
Short-term and Long-term Complications
Diabetes primarily causes long-term complications such as cardiovascular disease, neuropathy, nephropathy, and retinopathy due to chronic high blood sugar levels. Hypoglycemia, characterized by acute low blood sugar, can lead to short-term complications including confusion, seizures, loss of consciousness, and in severe cases, coma or death if not promptly treated. Preventing these complications requires tight glucose monitoring and management tailored to the specific risks associated with each condition.
Treatment and Management Strategies
Diabetes treatment focuses on maintaining blood glucose levels through insulin therapy, oral medications, and lifestyle changes like diet and exercise to prevent hyperglycemia complications. Hypoglycemia management requires immediate intake of fast-acting carbohydrates such as glucose tablets or juice, followed by a balanced meal to stabilize blood sugar and prevent recurrent episodes. Continuous monitoring of blood glucose levels is essential for both conditions to tailor treatment plans and reduce the risk of severe hypo- or hyperglycemic events.
Prevention Tips and Lifestyle Modifications
Effective diabetes and hypoglycemia prevention rely on balanced blood sugar management through a diet rich in fiber, whole grains, and lean proteins while minimizing refined sugars and processed foods. Regular physical activity enhances insulin sensitivity and stabilizes glucose levels, reducing the risk of both hyperglycemia and hypoglycemia episodes. Consistent meal timing and monitoring blood glucose levels enable early detection and adjustment to prevent dangerous blood sugar fluctuations.
When to Seek Medical Help
Seek medical help immediately if blood sugar levels fall below 70 mg/dL or if symptoms of hypoglycemia--such as sweating, confusion, or loss of consciousness--occur. For diabetes, urgent care is necessary when blood glucose exceeds 300 mg/dL, accompanied by symptoms like excessive thirst, frequent urination, or diabetic ketoacidosis signs. Timely medical intervention prevents severe complications, including seizures, coma, or long-term organ damage.
Diabetes Infographic
 libterm.com
libterm.com