Veracity is the quality of being truthful and accurate, essential for building trust in communication and data. Understanding veracity helps you evaluate the reliability of information sources and make informed decisions. Explore the rest of this article to discover how veracity impacts your daily interactions and critical assessments.
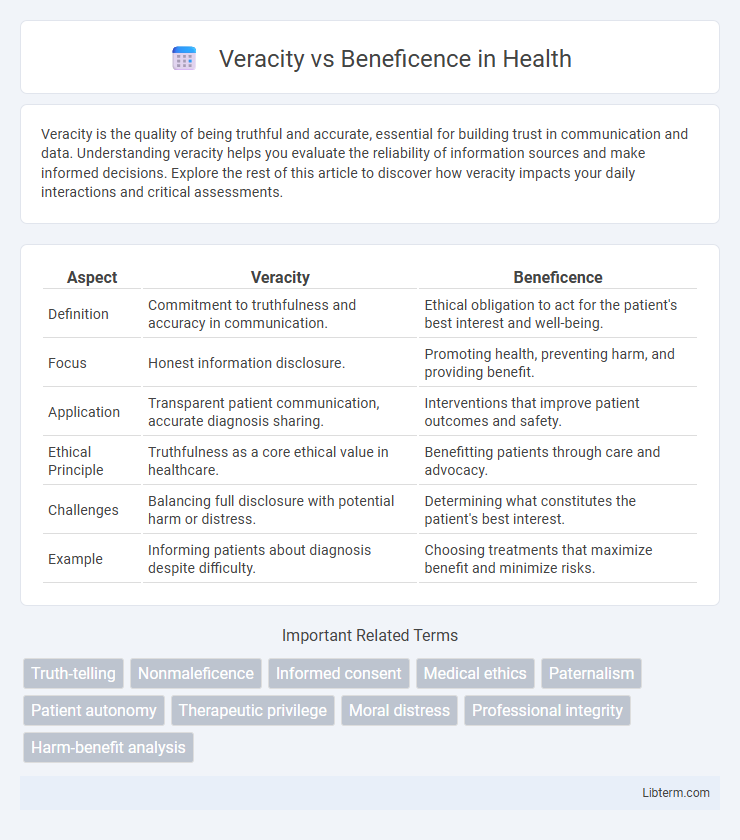
Table of Comparison
| Aspect | Veracity | Beneficence |
|---|---|---|
| Definition | Commitment to truthfulness and accuracy in communication. | Ethical obligation to act for the patient's best interest and well-being. |
| Focus | Honest information disclosure. | Promoting health, preventing harm, and providing benefit. |
| Application | Transparent patient communication, accurate diagnosis sharing. | Interventions that improve patient outcomes and safety. |
| Ethical Principle | Truthfulness as a core ethical value in healthcare. | Benefitting patients through care and advocacy. |
| Challenges | Balancing full disclosure with potential harm or distress. | Determining what constitutes the patient's best interest. |
| Example | Informing patients about diagnosis despite difficulty. | Choosing treatments that maximize benefit and minimize risks. |
Understanding Veracity in Healthcare
Veracity in healthcare emphasizes the ethical obligation of healthcare professionals to provide truthful and accurate information to patients, fostering trust and informed decision-making. Maintaining veracity involves transparent communication about diagnoses, treatment options, and potential risks, which is essential for preserving patient autonomy and promoting ethical clinical practice. Balancing veracity with beneficence requires careful consideration to ensure that honesty does not cause unnecessary harm while supporting patient well-being.
The Principle of Beneficence Explained
The Principle of Beneficence emphasizes acting in the best interests of others by promoting good, preventing harm, and providing benefits while minimizing risks. It requires healthcare professionals to prioritize patient welfare, making decisions that enhance well-being and support recovery. This principle often guides ethical medical practices, balancing positive outcomes against potential harm in clinical settings.
Key Differences Between Veracity and Beneficence
Veracity emphasizes the ethical obligation to tell the truth and provide accurate information, ensuring transparency and trust in interactions. Beneficence focuses on promoting the well-being and best interests of others, guiding actions that help prevent harm and enhance positive outcomes. The key difference lies in veracity prioritizing honesty, while beneficence centers on acting benevolently to benefit others, sometimes requiring delicate balance when truth-telling may conflict with the patient's welfare.
Historical Perspectives on Medical Ethics
Historical perspectives on medical ethics highlight the tension between veracity, the obligation to tell the truth, and beneficence, the duty to act in the patient's best interest. Early Hippocratic texts emphasized beneficence by advocating for patient welfare, often supporting non-disclosure to prevent harm, while modern bioethics increasingly prioritize veracity as essential for informed consent. Landmark cases and shifting cultural values throughout the 20th century underscored the evolution from paternalistic models towards transparency, balancing truth-telling with compassionate care.
Real-World Conflicts: Veracity vs Beneficence
Real-world conflicts between veracity and beneficence often arise in medical ethics when healthcare professionals must balance truth-telling with patient well-being, such as deciding whether to disclose a terminal diagnosis that may cause distress. Clinical scenarios demonstrate how strict adherence to veracity can undermine beneficence if full disclosure leads to anxiety or harm, while prioritizing beneficence might justify partial truth or deception to preserve hope and psychological stability. Ethical frameworks guide practitioners in navigating these tensions by evaluating patient autonomy, potential outcomes, and contextual factors to achieve a morally justified resolution.
Implications for Patient Care
Veracity in patient care ensures transparent and honest communication, fostering trust and informed decision-making, which enhances patient autonomy and satisfaction. Beneficence emphasizes acting in the patient's best interest by providing treatments that promote well-being and prevent harm, directly influencing clinical outcomes and ethical care standards. Balancing veracity and beneficence requires healthcare professionals to deliver truthful information compassionately while prioritizing therapies that maximize patient health benefits, thereby improving overall quality of care and patient adherence.
Ethical Frameworks Guiding Decision-Making
Veracity and beneficence are fundamental principles within ethical frameworks guiding decision-making, especially in healthcare and professional ethics. Veracity emphasizes truthfulness and transparency to maintain trust and informed consent, while beneficence focuses on actions that promote the well-being and best interests of individuals. Balancing these principles requires careful consideration of ethical theories such as deontology and utilitarianism to ensure decisions honor honesty without compromising the welfare of those affected.
Balancing Truth-Telling and Patient Welfare
Balancing veracity and beneficence requires healthcare providers to carefully navigate truth-telling while prioritizing patient welfare and emotional well-being. Transparent communication fosters trust but must be tailored to avoid causing unnecessary distress or harm. Ethical practice involves assessing individual patient needs to deliver honest information compassionately, ensuring informed decision-making and promoting optimal health outcomes.
Case Studies Highlighting Ethical Dilemmas
Case studies involving veracity versus beneficence often illustrate the conflict between truth-telling and acting in a patient's best interest. In oncology, disclosing a terminal diagnosis challenges practitioners to balance honesty with preserving patient hope, as seen in landmark cases like the Tarasoff decision influencing duty to warn. Ethical dilemmas arise when withholding information might protect emotional well-being but compromise informed consent, highlighting the complexity of applying these principles in clinical practice.
Promoting Ethical Integrity in Clinical Practice
Veracity and beneficence are fundamental ethical principles that promote integrity in clinical practice by ensuring honesty and prioritizing patient welfare. Upholding veracity involves transparent communication and truthful disclosure, fostering trust and informed decision-making between clinicians and patients. Beneficence drives healthcare providers to act in the best interest of patients, balancing truth-telling with compassionate care to optimize clinical outcomes and uphold professional ethics.
Veracity Infographic
 libterm.com
libterm.com