Hypocapnia refers to an abnormally low level of carbon dioxide in the blood, often caused by rapid or deep breathing known as hyperventilation. This condition can lead to symptoms such as dizziness, tingling sensations, and muscle cramps due to the imbalance of oxygen and carbon dioxide in your body. Discover more about the causes, symptoms, and treatments of hypocapnia by reading the full article.
Table of Comparison
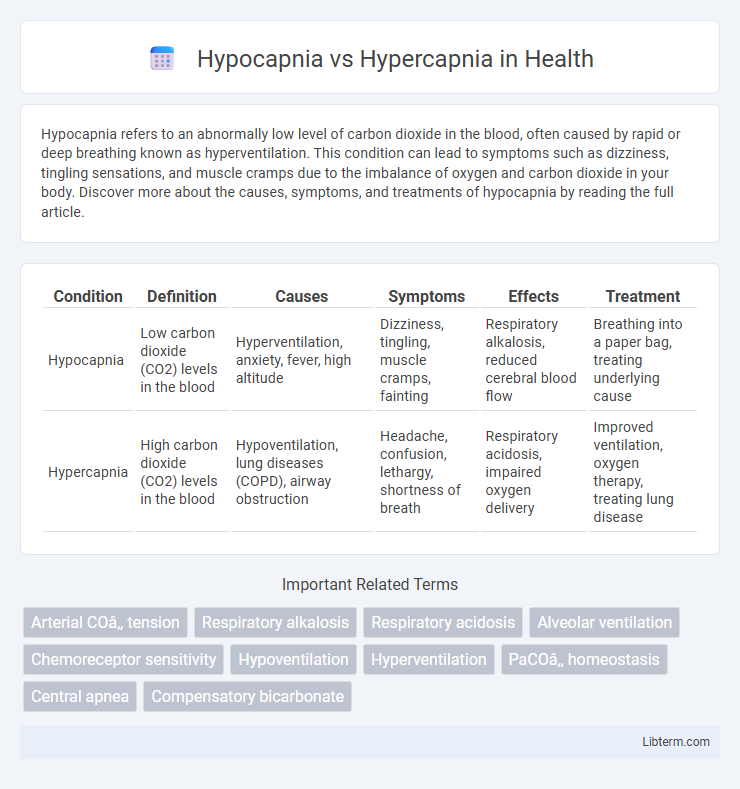
| Condition | Definition | Causes | Symptoms | Effects | Treatment |
|---|---|---|---|---|---|
| Hypocapnia | Low carbon dioxide (CO2) levels in the blood | Hyperventilation, anxiety, fever, high altitude | Dizziness, tingling, muscle cramps, fainting | Respiratory alkalosis, reduced cerebral blood flow | Breathing into a paper bag, treating underlying cause |
| Hypercapnia | High carbon dioxide (CO2) levels in the blood | Hypoventilation, lung diseases (COPD), airway obstruction | Headache, confusion, lethargy, shortness of breath | Respiratory acidosis, impaired oxygen delivery | Improved ventilation, oxygen therapy, treating lung disease |
Introduction to Blood CO2 Levels
Hypocapnia refers to abnormally low levels of carbon dioxide (CO2) in the blood, typically below 35 mmHg, while hypercapnia indicates elevated CO2 concentrations, usually above 45 mmHg. Blood CO2 levels are tightly regulated because CO2 plays a critical role in maintaining acid-base balance and proper respiratory function. Disruptions in CO2 homeostasis can lead to respiratory alkalosis in hypocapnia or respiratory acidosis in hypercapnia, impacting cellular metabolism and oxygen delivery.
What is Hypocapnia?
Hypocapnia is a condition characterized by abnormally low levels of carbon dioxide (CO2) in the blood, typically below 35 mmHg. It often results from hyperventilation, leading to respiratory alkalosis and decreased cerebral blood flow. Monitoring arterial CO2 tension is critical in diagnosing and managing hypocapnia to prevent neurological and cardiovascular complications.
What is Hypercapnia?
Hypercapnia is a medical condition characterized by elevated levels of carbon dioxide (CO2) in the bloodstream, often resulting from hypoventilation or impaired lung function. This increase in arterial CO2 partial pressure (PaCO2) can cause respiratory acidosis and lead to symptoms such as headache, confusion, and shortness of breath. In contrast to hypocapnia, which involves reduced CO2 levels, hypercapnia signifies a critical imbalance in respiratory gas exchange requiring prompt diagnosis and treatment.
Causes of Hypocapnia
Hypocapnia is primarily caused by hyperventilation, which leads to excessive expulsion of carbon dioxide from the bloodstream, often triggered by anxiety, pain, or metabolic acidosis. Other causes include lung diseases such as pneumonia or pulmonary embolism that result in increased respiratory rates and reduced carbon dioxide levels. Understanding these causes is crucial for managing respiratory alkalosis associated with hypocapnia.
Causes of Hypercapnia
Hypercapnia, characterized by elevated carbon dioxide levels in the blood, typically results from hypoventilation caused by respiratory conditions such as chronic obstructive pulmonary disease (COPD), severe asthma, or neuromuscular disorders that impair respiratory muscle function. Other causes include central nervous system depression due to drug overdose, obesity hypoventilation syndrome, and acute respiratory failure. In contrast, hypocapnia arises from excessive alveolar ventilation leading to decreased arterial CO2, often triggered by hyperventilation due to anxiety, pain, or metabolic disturbances.
Clinical Manifestations of Hypocapnia
Hypocapnia typically presents with symptoms such as dizziness, lightheadedness, numbness or tingling in the extremities, and muscle cramps due to decreased carbon dioxide levels in the blood causing respiratory alkalosis. Patients may also experience chest pain, palpitations, and shortness of breath, often linked to hyperventilation. Severe hypocapnia can lead to cerebral vasoconstriction, resulting in confusion, syncope, or seizures.
Clinical Manifestations of Hypercapnia
Hypercapnia presents with clinical manifestations including headache, confusion, flushed skin, and lethargy due to elevated arterial carbon dioxide levels. Severe hypercapnia may lead to respiratory acidosis, increased intracranial pressure, and altered mental status, potentially progressing to coma. Early recognition of symptoms such as dyspnea, tachypnea, and muscle twitching is critical for prompt intervention and management.
Diagnostic Methods for CO2 Imbalance
Diagnostic methods for CO2 imbalance prioritize arterial blood gas (ABG) analysis to accurately measure partial pressure of carbon dioxide (PaCO2), essential in distinguishing hypocapnia (PaCO2 < 35 mmHg) from hypercapnia (PaCO2 > 45 mmHg). Capnography provides continuous, non-invasive monitoring of end-tidal CO2 (ETCO2), reflecting real-time ventilation status and aiding in rapid detection of CO2 imbalances. Pulmonary function tests alongside clinical assessment enhance the evaluation of underlying respiratory disorders contributing to aberrant CO2 levels.
Treatment Approaches for Hypocapnia and Hypercapnia
Treatment approaches for hypocapnia primarily involve addressing the underlying cause of reduced carbon dioxide levels, such as anxiety or hyperventilation, often through controlled breathing techniques and rebreathing into a paper bag to restore normal CO2 balance. Hypercapnia treatment focuses on improving ventilation to increase carbon dioxide elimination, including the use of non-invasive positive pressure ventilation (NIPPV) or mechanical ventilation in severe cases of respiratory failure. Managing the underlying respiratory conditions like chronic obstructive pulmonary disease (COPD) or acute respiratory distress syndrome (ARDS) is critical in both hypocapnia and hypercapnia to restore normal blood gas levels.
Prevention and Management Strategies
Hypocapnia, characterized by abnormally low carbon dioxide levels in the blood, can be prevented by controlled breathing techniques and addressing underlying causes such as anxiety or pain. Hypercapnia, involving elevated carbon dioxide levels, requires management strategies like improving ventilation through noninvasive or invasive mechanical support and treating respiratory conditions such as COPD or sleep apnea. Monitoring arterial blood gases regularly enables timely intervention to maintain optimal CO2 levels and prevent complications.
Hypocapnia Infographic
 libterm.com
libterm.com